Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Arthrocentesis is typically performed on patients with an acutely inflamed joint of unclear etiology. This is most often done to rule out septic arthritis, especially in patients with a red, swollen, and painful joint.
In the absence of a positive gram stain, an elevated synovial fluid (SF) white count of >25,000 is usually suggestive of an infected joint. However, there does not appear to be a reliable cut off to make a diagnosis of septic arthritis. Missing a diagnosis or a delay in the treatment can lead to extensive damage to the articular cartilage. Hence making an early diagnosis is especially important.
Artificial intelligence (AI) applications in healthcare have seen a steady rise over the past decade. Machine learning and deep learning models have been extensively used to discover patterns and predict patient outcomes. AI applications have shown promise in a number of fields, from radio diagnostics to infectious diseases. Our study was aimed at developing and accessing a machine learning model to predict the likelihood of septic arthritis before synovial fluid culture results are available.
Methods:
- We retrospectively collected data on 98 patients that had synovial fluid aspirations done at our community hospital over a 4-year period. A diagnosis of septic arthritis was confirmed based on the results of the synovial cultures on day 5.
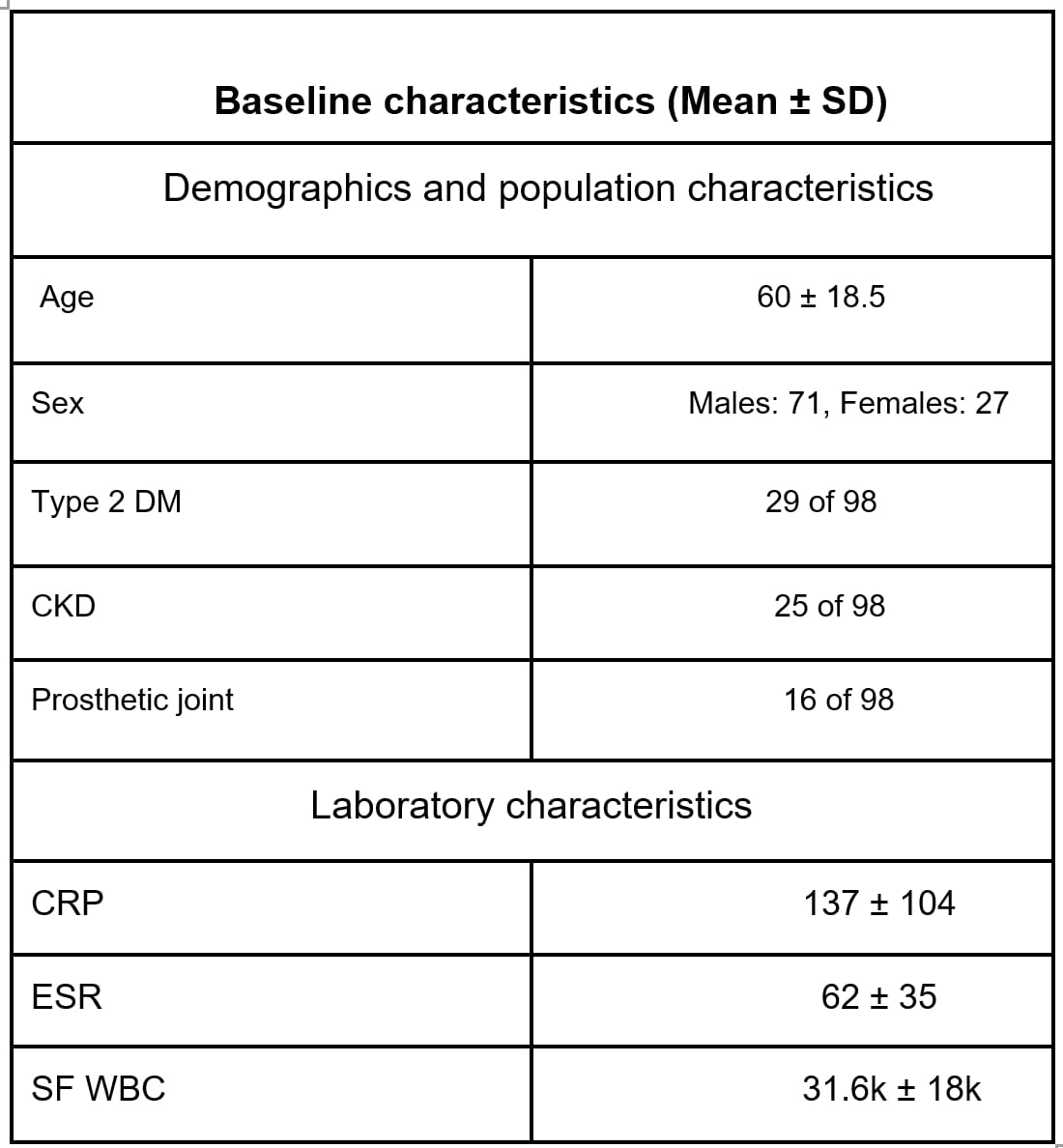
- Medical history, presenting clinical features, and corresponding laboratory values were recorded (Fig 1).
- Prior to building the model, the data was preprocessed and normalized. Boolean values were converted to binary representations and categorical features were converted to numerical values.
- The dataset was then split into a training and test set, with an 80:20 randomly sampled split.
- A Random Forest Classifier algorithm was used to build the model, which was then evaluated using the test set.
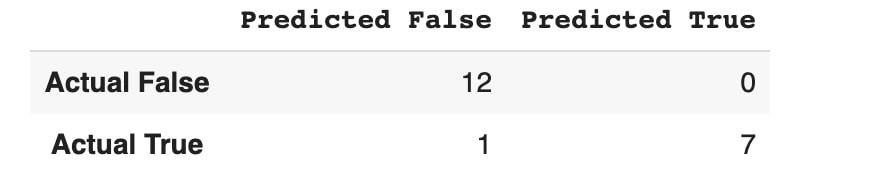
- Feature importance was plotted, and a confusion matrix generated to view the false positives/negative count (Fig 2).
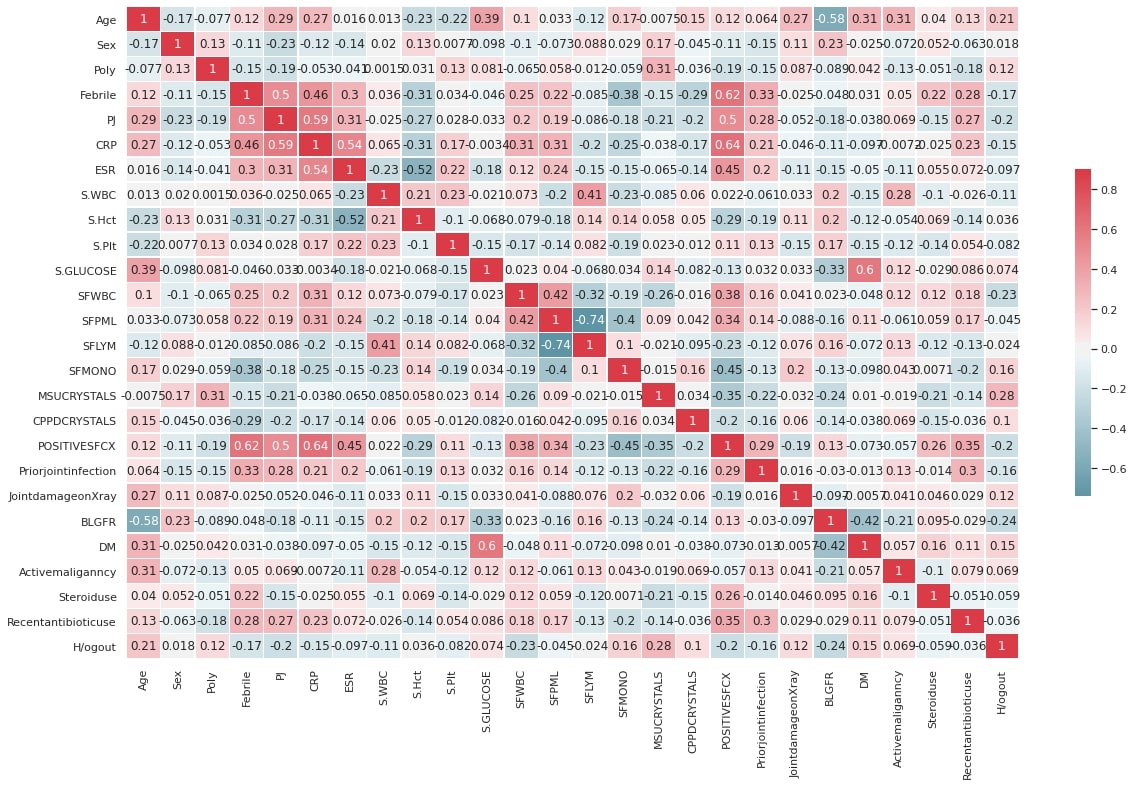
- Finally, column correlations were generated using a heatmap (Fig. 3) to explore the data and validate the features that the model had selected.
Results:
- In total, 33 of the 98 (33.6%) SF cultures came back positive.
- The most common organism identified was methicillin-sensitive staphylococcus aureus (42% of positive cultures).
- 22 of the 65 patients (33.8%) with ultimately negative cultures were empirically started on antibiotics at presentation, while, 3 of the 33 patients (9%) with positive cultures had not been initiated on antibiotics.
- Our feature importance plot indicated that CRP and SF monocytes were the strongest positive and negative predictors of SA, respectively.
- When evaluated with the test set, our prediction model proved to be quite accurate with a sensitivity of 87% and a specificity of 100% (accuracy of 95%).
Conclusion: Our proof of concept indicated that it is possible to build a well-performing model to predict septic arthritis cases using machine learning. With a larger sample size, more robust methods can be leveraged for predictive modeling and higher performance and accuracy. Ultimately, the output can be used to generate a risk score to determine a patient’s likelihood of septic arthritis.
To cite this abstract in AMA style:
Gilvaz V, Mody E, Rapose A, Radhakrishnan S, Abaalkhail S, Vibhavari Guntupalli S. Machine Learning Model to Predict Culture Positivity in Suspected Septic Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/machine-learning-model-to-predict-culture-positivity-in-suspected-septic-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/machine-learning-model-to-predict-culture-positivity-in-suspected-septic-arthritis/