Session Information
Date: Sunday, November 8, 2015
Title: Osteoporosis and Metabolic Bone Disease - Clinical Aspects and Pathogenesis Poster
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
There is an evidence
vacuum concerning the mechanisms underlying the high atherosclerotic cardiovascular
disease (ASCVD) burden in patients with psoriatic arthritis (PsA). In the
general population, osteoporosis and low bone mineral density (BMD) are risk
factors for ASCVD. However, this has not been established for patients with PsA.
The T-score represents a patient’s BMD compared to the BMD of a healthy 30-year
old and is the most commonly used measure when screening for osteoporosis. The
aim of the present study was to evaluate if low BMD, measured by T-score, is correlated
with ASCVD in patients with PsA.
Methods:
In this cross-sectional
study, patients with PsA, recruited from an outpatient clinic, underwent a thorough
clinical rheumatology examination, carotid ultrasound, laboratory tests and BMD
measurements by dual-energy X-ray absorptiometry (DXA) scans. Established ASCVD
was defined as a previous ASCVD event (acute myocardial infarction, coronary
interventions, transient ischemic attack [TIA] and ischemic stroke),
established peripheral artery disease or atherosclerotic carotid artery plaque(s).
Unadjusted and adjusted analyses of variance (ANOVA) were applied to compare
the T-score between patients with and without ASCVD. In addition, we performed
logistic regression analyses with ASCVD as the dependent variable, both unadjusted
and adjusted (age, gender and BMI) and evaluated the Nagelkerke R2 as
a proxy for the degree of correlation between ASCVD and T-score, traditional
CVD risk factors, inflammatory biomarkers and PsA disease activity variables.
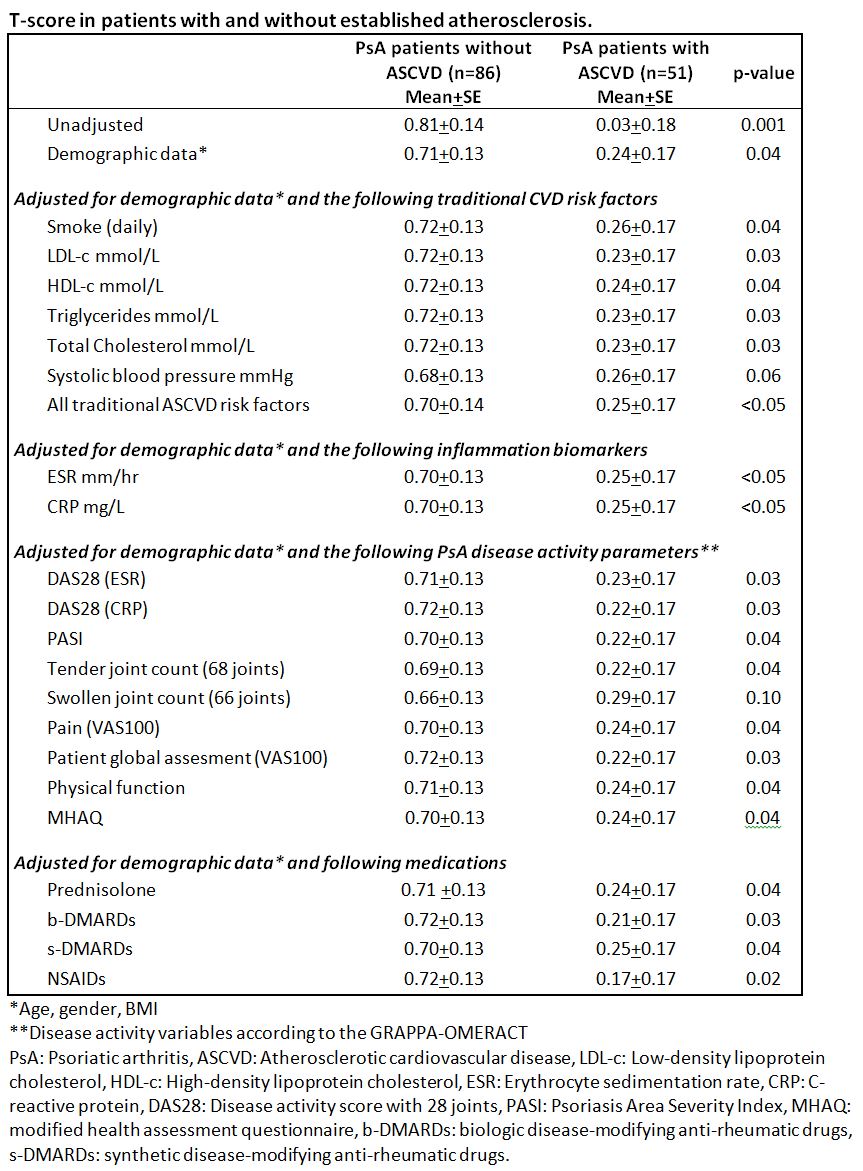
male and the median (IQR) age and disease duration was 53.0 (44.5, 59.5) and
7.8 (3.2, 12.5) years, respectively. The T-score was significantly lower in
patients with ACVD compared to those without (p=0.001) (Table). This finding
was largely robust to adjustments for demographic data (p=0.04), traditional
CVD risk factors (p=0.03-0.06), inflammatory biomarkers (p<0.05), PsA
disease activity (p=0.03-0.10) and common rheumatology drugs (p=0.02-0.04). In
logistic regression analyses with ASCVD as the dependent variable, the
Nagelkerke R2 value for T-score (unadjusted: 0.11, adjusted: 0.27)
was higher than for ACVD risk factors (unadjusted: 0.003-0.04, adjusted: 0.23-0.25),
inflammatory biomarkers (unadjusted: 0.005-0.05, adjusted: 0.24) and PsA
disease activity variables (unadjusted: <0.001-0.04, adjusted: 0.23-0.26).
Conclusion:
provides the first evidence of an association between ACVD and low BMD in PsA
patients, which was robust to adjustments. In addition, ACVD was more strongly
correlated with the T-score than with traditional CVD risk factors, inflammatory
biomarkers or PsA disease activity. Our results suggest that there may be
indication for CVD risk evaluation including carotid ultrasound in PsA patients
with low BMD.
To cite this abstract in AMA style:
Ikdahl E, Kilander Høiberg H, Rollefstad S, Diamantopoulos AP, Wibetoe G, Kavanaugh A, Olsen IC, Kvien TK, Semb AG, Haugeberg G. Low Bone Density Is Associated with Atherosclerotic Disease in Patients with Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/low-bone-density-is-associated-with-atherosclerotic-disease-in-patients-with-psoriatic-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/low-bone-density-is-associated-with-atherosclerotic-disease-in-patients-with-psoriatic-arthritis/