Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Renal involvement is common in ANCA-associated vasculitis (AAV). Prior analyses show that end stage renal disease (ESRD) in AAV may be multifactorial. Little is known about the longitudinal course of renal dysfunction in contemporary AAV cohorts. We aimed to identify renal function trajectories using an unbiased approach, and to assess the baseline comorbidities and outcomes associated with these trajectories.
Methods: Patients with a baseline creatinine (30-365 days before treatment initiation) were included from the Mass General Brigham AAV Cohort, a consecutive inception cohort (2002-2017). Follow-up began 1 year before and was truncated 10 years after treatment initiation. Treatment resistance was defined as lack of remission following the first course of therapy; remission was defined by stabilization or improvement of estimated glomerular filtration rate (eGFR) without hematuria for ≥1 month. In patients without repeat urinalysis, stabilization or improvement of eGFR was considered evidence of remission.
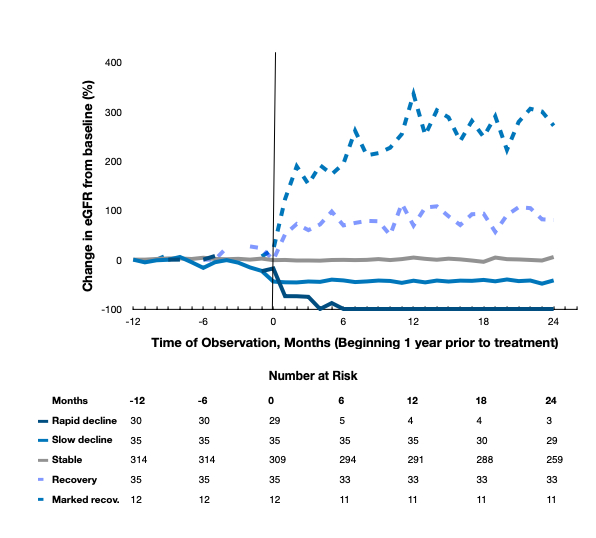
We calculated eGFR using CKD-EPI without race multiplier. We used trajectory analysis to identify groups with similar longitudinal change in renal function, defined as percentage of pre-AAV eGFR over the first 24 months of follow up. Final models were selected by fit statistics and face validity.
ESRD was defined as (1) need for dialysis for >60 days, (2) dialysis until death if the patient died between 14-60 days of follow up, or (3) renal transplant, as identified by chart review and United States Renal Data System records. Logistic regression was used to evaluate risk factors for trajectory group membership, and Cox proportional hazards models were used to estimate risk of ESRD in each trajectory group, accounting for competing risk of death.
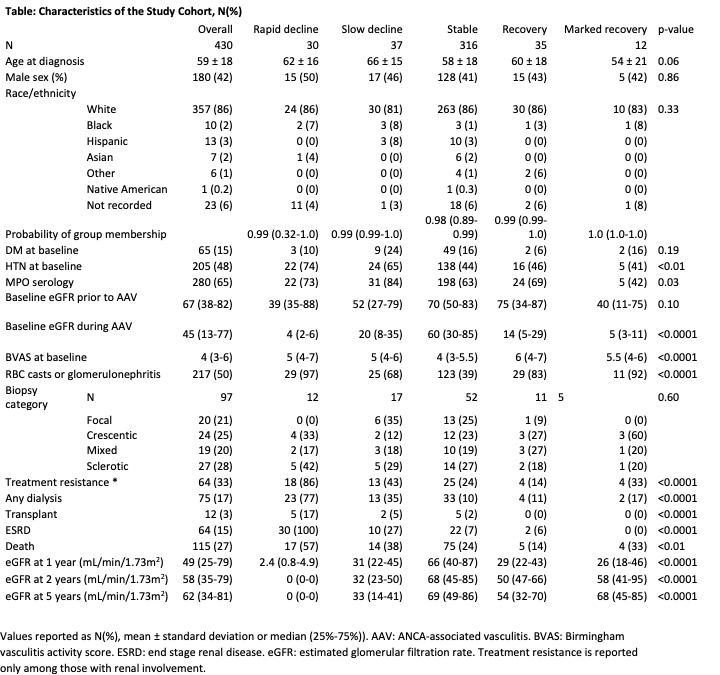
Results: Of 484 patients in the cohort, 430 were included. We identified 5 groups (Figure): rapid decline (RD) (N=30), slow decline (SD) (N=37), stable (N=316), recovery (N=35) and marked recovery (N=12). The median posterior probability of group membership was >0.98 in all groups, indicating excellent fit.
Age, sex, race and biopsy class were overall similar between groups; however, RD and SD groups tended to be older than those with a stable course, and sclerotic biopsy classification was most common among RD. MPO serology and hypertension (HTN), but not diabetes (DM), were more common in RD and SD than other groups (Table). Treatment resistance was more common in RD than SD (86% vs 43%, p< 0.001), and more common in these groups than in the stable and recovery groups.
In a logistic model adjusted for age and ANCA type, baseline HTN (OR 2.3, 95% CI 1.3-4.4) but not DM (OR 0.9, 95%CI 0.4-1.8) was associated with odds of membership in RD or SD groups versus any other group. In an age-adjusted model, the RD and SD groups had a higher risk of ESRD compared to the stable group (HR 647, 95%CI 128-377 and HR 14, 95%CI 4-46, respectively).
Conclusion: In a large AAV cohort, we identified distinct patterns of change in renal function. Baseline HTN was associated with a worse trajectory and treatment resistance was more common among those with a worse trajectory. Both RD and SD groups were associated with higher risk of ESRD.
To cite this abstract in AMA style:
Hanberg J, Fu X, Cook C, Stone J, Choi H, Wallace Z. Longitudinal Patterns of Renal Function in ANCA-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/longitudinal-patterns-of-renal-function-in-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-patterns-of-renal-function-in-anca-associated-vasculitis/