Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Our group has developed a conceptual model to categorize SLE manifestations into two dimensions termed Type 1 and Type 2. Type 1 SLE consists of active inflammatory manifestations like arthritis, nephritis, and rashes, and Type 2 SLE includes symptoms of fatigue, myalgia, mood disturbance, and cognitive dysfunction. SLE is characterized by waxing and waning of Type 1 inflammatory features considered to be disease activity. To advance lupus symptom characterization, we assessed whether Type 2 symptoms fluctuate over time.
Methods: SLE patients meeting SLICC criteria with ≥2 visits at a university rheumatology clinic between January 2018 and May 2019 were included. At each visit, SLEDAI was measured and patients completed the ACR FM Diagnostic Criteria. The FM severity score (FSS) is the sum of the widespread pain (0-19) and symptom severity scores (0-12). Patients were classified as having Type 1 SLE manifestations (SLEDAI ≥6, clinical SLEDAI ≥4, or active nephritis), Type 2 SLE symptoms (FSS >10), Mixed (both Type 1 and Type 2), or Minimal (neither Type 1 or Type 2). A clinically significant change in SLEDAI and FSS was defined as a +/- 2-point change between two visits for either of these measures. Changes in Type 1 and Type 2 severity between the two visits were estimated using simple statistics.
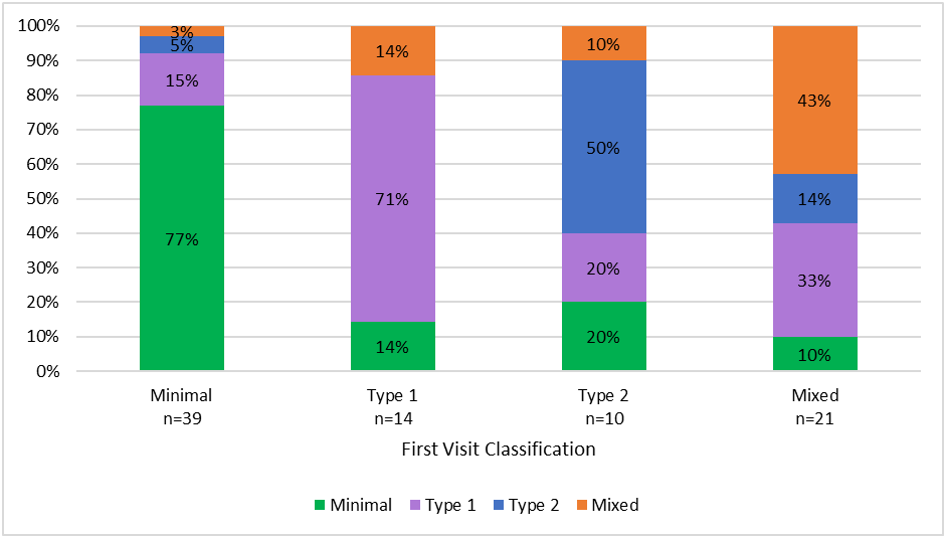
Results: 84 patients were included in the analysis (mean age 42 years, mean duration of SLE 14 years, 95% female, 65% African American, 56% with history of lupus nephritis). The average time between visits was 19 weeks (range: 4-34). At the first visit, 17% of patients were classified as Type 1, 12% as Type 2, 25% as Mixed, and 46% as Minimal. In patients with Minimal or Type 1 SLE at Visit 1, 8-14% experienced active Type 2 symptoms at Visit 2 (Figure 1). In comparison, for patients with Type 2 or Mixed SLE at Visit 1, approximately 40% were no longer classified as having active Type 2 symptoms at Visit 2.
Overall, 44% of patients had an improved FSS at Visit 2 and 30% had improvement in SLEDAI (Figure 2). Type 2 symptoms fluctuated in all patient groups between visits. Type 2 SLE symptoms worsened in 21% of Minimal and 36% of Type 1 SLE patients. Interestingly, patients with Mixed activity appeared to have a greater improvement in FSS (81%) compared to patients with only Type 2 SLE activity (50%). When specific Type 2 symptoms were explored, 78% of patients who reported moderate or severe fatigue at Visit 1 continued to have moderate or severe fatigue at Visit 2, whereas only 16% of patients without fatigue at Visit 1 experienced fatigue at Visit 2. Fatigue was more prevalent and persistent in patients classified as Type 2 and Mixed at Visit 1. Improvements were seen in cognitive dysfunction, muscle weakness, and muscle pain, with approximately 40% of patients reporting improvement in symptoms at Visit 2.
Conclusion: Our findings suggest that, similar to Type 1 features, Type 2 symptoms vary over time, with almost half of the patients in the analysis having an improvement in FSS between visits. Future studies are needed to determine Type 2 fluctuations over a longer follow-up period, as well as to identify treatment approaches to improve Type 2 symptoms.
The bars represent the distribution of patient symptoms at Visit 2 for each Visit 1 classification group.
To cite this abstract in AMA style:
Eudy A, Rogers J, Whitney R, Criscione-Schreiber L, Doss J, Pisetsky D, Sadun R, Sun K, Clowse M. Longitudinal Changes in Manifestations of SLE [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/longitudinal-changes-in-manifestations-of-sle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-changes-in-manifestations-of-sle/