Session Information
Date: Wednesday, November 13, 2019
Title: 6W017: Health Services Research II: Health Economics (2888–2893)
Session Type: ACR/ARP Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: The United States (US) knee osteoarthritis (OA) population has low levels of physical activity (PA), despite its well-defined health benefits. Interventions to promote PA are often stymied by concerns of lack of sustainability of intervention efficacy. We sought to evaluate lifetime benefits and cost-effectiveness of a short term (3-year) PA intervention in this population.
Methods: Using the validated computer microsimulation Osteoarthritis Policy Model, we examined the long-term clinical and economic impacts of a 3-year PA intervention for inactive adults, aged 55(5) (mean(SD)), with knee OA. The PA program was concurrent with standard of care (SOC), which included non-pharmacologic, pharmacologic, and surgical guideline-based regimens. The PA intervention, based on the SPARKS (Studying Physical Activity Rewards after Knee Surgery) trial, cost $287/person-year and incorporated wearable activity monitors, health coaching, and financial incentives for reaching predetermined PA goals. We considered 3 PA levels: inactive (< 30 minutes of moderate-to-vigorous PA/week), insufficiently active (30-149 min/week), and active (150+ min/week). Intervention efficacy was derived from the SPARKS data as the probability of increasing PA by at least one level, estimated as 0.38. We used accelerometry data from the Osteoarthritis Initiative to derive the impact of PA level on quality of life (QoL). Annual background medical cost savings for active ($714) and insufficiently active ($313) persons and reduction in incidence of cardiovascular disease (CVD) and type 2 diabetes mellitus (DM) compared to inactive persons were derived from the published literature. In sensitivity analyses we varied PA program cost, impact of PA on QoL, and PA-related background medical costs. All cost and QoL results were discounted by 3% annually. Cost-effectiveness of the PA program was defined using incremental cost-effectiveness ratios (ICERs), calculated as the difference in cost over the difference in accrued quality-adjusted life-years (QALYs) due to the PA program. This analysis was conducted from a healthcare systems perspective.
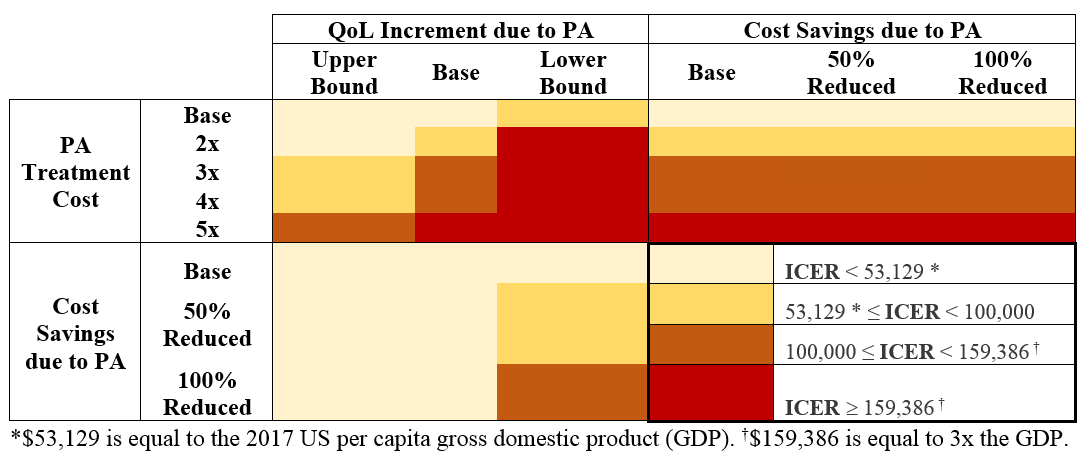
Results: The addition of a 3-year PA intervention to SOC for inactive adults with knee OA had an ICER of $16,000/QALY. Participation of 10% of the estimated 4 million inactive US adults with knee OA in such a program could prevent 212 cases of CVD and 319 cases of DM and save 7,476 quality-adjusted life years. Increasing cost of the PA program by 4x raised the ICER to $152,000/QALY (< 3x the US gross domestic product); varying QoL increment due to PA yielded ICERs from $10,000-58,000/QALY; varying background cost due to PA did not qualitatively affect ICERs. Results of two-way sensitivity analyses are presented in the Figure. Offering this program to all US adults with knee OA, regardless of baseline PA, yielded an ICER of $42,000/QALY.
Conclusion: A short-term PA intervention with no sustainability of efficacy beyond a 3-year time horizon in the knee OA population is cost-effective. Given its cost-effectiveness and clinical benefits, providers and payers may consider incorporating a PA intervention into usual care of knee OA patients.
To cite this abstract in AMA style:
Silva G, Sullivan J, Katz J, Messier S, Losina E. Long-term Clinical and Economic Benefits of a Short-term Physical Activity Intervention Among Inactive Knee Osteoarthritis Patients in US: A Model-based Evaluation [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/long-term-clinical-and-economic-benefits-of-a-short-term-physical-activity-intervention-among-inactive-knee-osteoarthritis-patients-in-us-a-model-based-evaluation/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-clinical-and-economic-benefits-of-a-short-term-physical-activity-intervention-among-inactive-knee-osteoarthritis-patients-in-us-a-model-based-evaluation/