Session Information
Date: Tuesday, November 7, 2017
Title: Rheumatoid Arthritis – Clinical Aspects Poster III: Comorbidities
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Over the past two decades, the use of disease modifying anti-rheumatic drugs and treat-to-target strategies have dramatically improved the outcomes of patients with rheumatoid arthritis (RA). This has led to a decline in the rate of joint surgery, which is traditionally reserved for treatment of refractory patients aiming to improve function and quality of life. The goal of this study was to identify risk factors for joint surgery in RA and assess trends in surgery rates over time.
Methods: A retrospective medical record review was performed of all orthopedic surgeries following first fulfilment of 1987 ACR criteria for adult-onset RA in 1980-2013 among residents of a geographically defined area with follow up until death, migration or July 1, 2016. Surgeries were classified as small (wrist, hand, foot) or large (shoulder, elbow, hip, knee, ankle) joint. Risk factors were examined using Cox models adjusted for age, sex and calendar year of RA incidence.
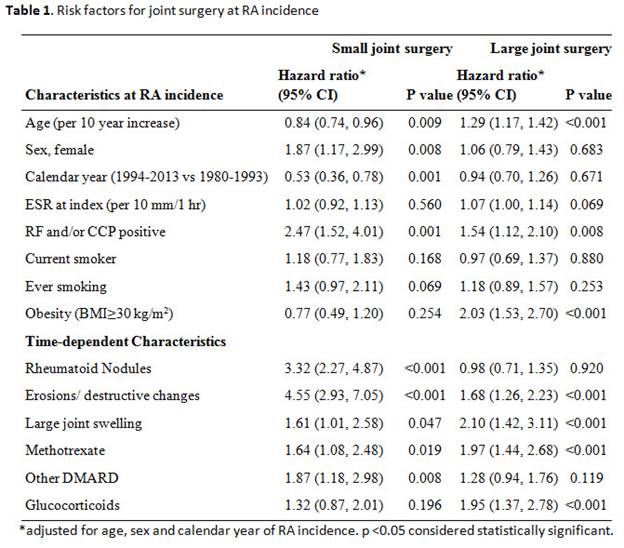
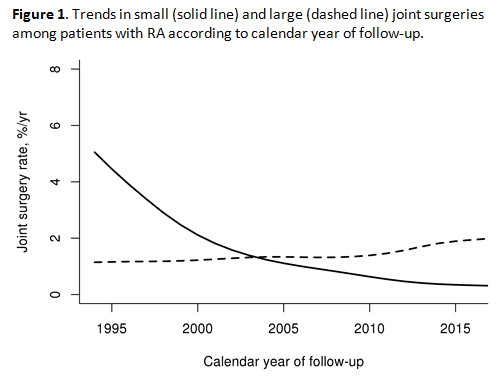
Results: A total of 1077 patients with RA (mean age (±SD) 55.9±15.6 years, 69% female, 66% RF and/or ACPA positive) were followed for a median follow-up of 10.7 years during which 112 and 204 underwent at least one joint small and large joint surgery, respectively. Results of risk factor analysis for joint surgery at RA incidence and during follow up are shown in table 1. Advanced age (per 10 year increase) was associated with an increased risk for both small joint surgery (SJS) and large joint surgery (LJS). Other significant risk factors at the time of RA incidence included rheumatoid factor and anti-CCP antibody positivity for both SJS and LJS, and BMI≥30 kg/m2 for LJS. Significant risk factors for SJS and LJS at any time during follow-up included the presence of radiographic erosions or destructive changes, large joint swelling, and methotrexate use. The use of glucocorticoids was associated with increased risk of LJS only. There was a decreased rate of SJS by calendar year of incidence (1994-2013 vs 1980-1993) (hazard ratio 0.53; p=0.001), and a significant decline in SJS incidence after 1995 with less than 1% of patients having surgery each year by the end of the study period (Figure). There were no significant trends in LJS over time.
Conclusion: There has been a significant decline in the incidence of SJS in RA but no change in the rate of LJS. Positive serologies, rheumatoid nodulosis, and radiographic erosions are strong predictors for SJS, but are also associated with increased risk for LJS. Increasing age and obesity are predictive of LJS, similar to the general population.
To cite this abstract in AMA style:
Richter M, Crowson CS, Matteson EL, Makol A. Joint Surgery in Rheumatoid Arthritis 1980-2013: A Population-Based Study to Identify Risk Factors and Time Trends in Incidence [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/joint-surgery-in-rheumatoid-arthritis-1980-2013-a-population-based-study-to-identify-risk-factors-and-time-trends-in-incidence/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/joint-surgery-in-rheumatoid-arthritis-1980-2013-a-population-based-study-to-identify-risk-factors-and-time-trends-in-incidence/