Session Information
Title: Rheumatoid Arthritis - Clinical Aspects: Novel Biomarkers and Other Measurements of Disease Activity
Session Type: Abstract Submissions (ACR)
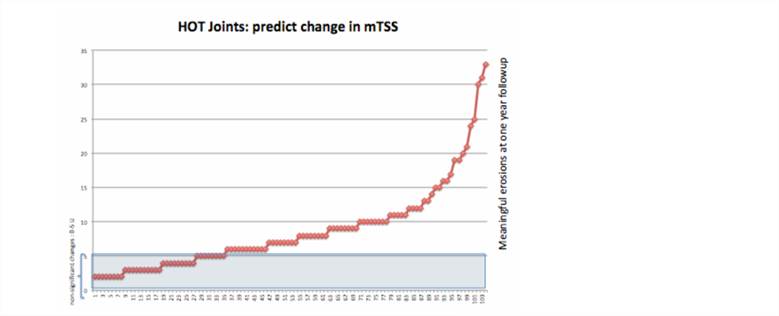
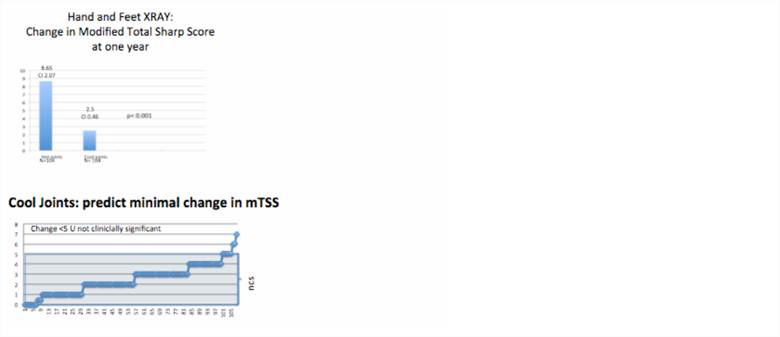
Background/Purpose: Joint dermal temperature (temp) measured in less than a minute can identify specifically the individual RA patient most likely to develop radiographic change on Sharp Score in the next year. There is great debate regarding which patients should be treated with expensive therapies for rheumatoid arthritis (RA). Certain subsets of RA patients are more likely to cripple, such as sero-positive disease, those earlier in disease onset, and earlier age at onset, and higher inflammatory non-specific markers (like amyloid, fibrinogen). However, can we identify a specific patient at most risk for radiographic changes. We evaluated the power of touch to determine disease. It has long been noted in the literature that skin over a gout joint is “hot”, which we define as a temp equal to or above central temp. Elevated skin temps occur also over septic joints and RA. The hot joint will identify which individual is destined for new xray erosions.
Methods: A digital clinic dermal thermometer was used to record vital signs, both at skin on the forehead and over any painful joint, most often the wrist. The dermal temp can be measured accurately and in less than a minute (accuracy ±0.1 F). Sequentially 208 sero-positive RA patients on MTX (15-25 mg/week) and with baseline plus one year follow up hand/feet xrays were enrolled. No biologic therapy was permitted. Xrays were scored by a single reader (MG) with a modified van der Heijde total Sharp score (mTSS) without sequence order or identifiers. Medical history, WESR, CRP, baseline medications and xray were performed at screening. A small group of subjects without RA (n=25) were used as controls to evaluate the usual range of joint temp.
Results: The dermal temp at a wrist of normal persons without RA is -12.0±4.6 F. The “hot” joint RA group had a joint temp in excess of central temp +1.06±0.69 (CI 0.23) and neared a 4-fold higher individual risk of new erosions compared to those RA “cool” joints. Results were highly significant, p<0.001. Sensitivity for joint temp predicting erosions is 91.7% and specificity for joint temp predicting erosions 78%. Newer onset of RA, younger age, and WESR were mildly significant (P<0.05) but had poor specificity and sensitivity.
Conclusion: A simple dermal temperature taken with a standard digital thermometer can quickly and accurately identify RA patients who are at high risk for further destructive change on MTX alone. This can be submitted to insurers, national health registries, and provides objective data to what we have known for centuries, that the human hand can detect active disease.
Disclosure:
M. Greenwald,
None;
J. Ball,
None;
H. Paulus,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/joint-dermal-temperature-specifically-identifies-the-individual-ra-patient-most-likely-to-develop-radiographic-change-on-sharp-score-an-exam-in-less-than-a-minute-can-predict-who-specifically-needs-b/