Session Information
Date: Monday, November 6, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Pathogenesis, Etiology Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Recent data has revealed occurrence of musculoskeletal manifestations in particular sacroiliitis and inflammatory back pain (IBP) secondary to isotretinoin therapy for acne valgaris, accordingly our study conducted to detect the prevalence of isotretinoin triggered rheumatic side-effects, with close clinical and radiological follow up to assess the drug impact on musculoskeletal system.
Methods:
513 acne patients on isotretinoin therapy were enrolled from dermatology out patients’ clinic, screened for musculoskeletal manifestations related features resulting from isotretinoin therapy, all patients were HLA B27 negative. At baseline C-reactive protein (CRP), Magnetic resonance imaging (MRI) sacroiliac joint, onset of IBP and pain score were reported. MRI proven sacroiliitis, has been scored with semi-quantitative score. Clinical and radiological follow up of our patients were done, patients who met ASAS classification criteria for spondyloarthropathy (SpA) were assessed for disease activity by Ankylosing Spondylitis Disease Activity Score (ASDAS) (3). MRI for sacroiliac joints and CRP were repeated three weeks after being symptomless, with isotretinoin discontinuation.
Results:
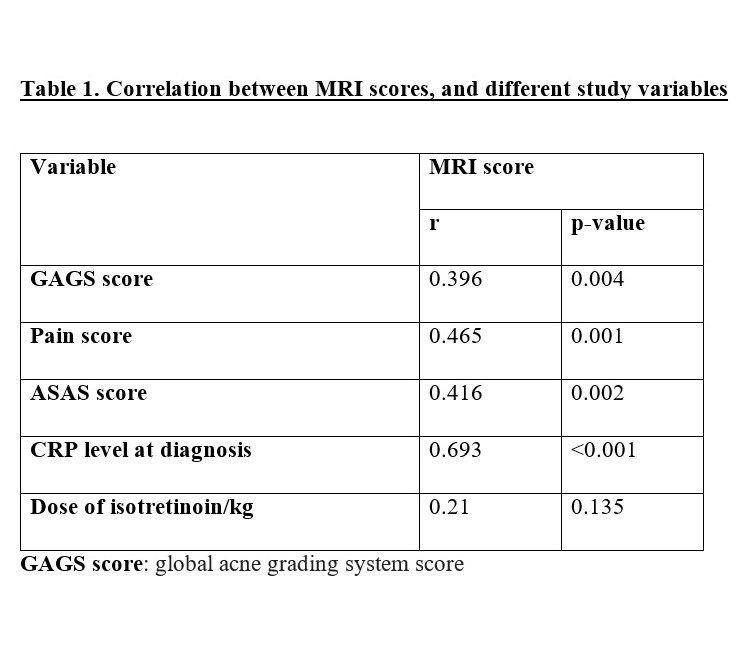
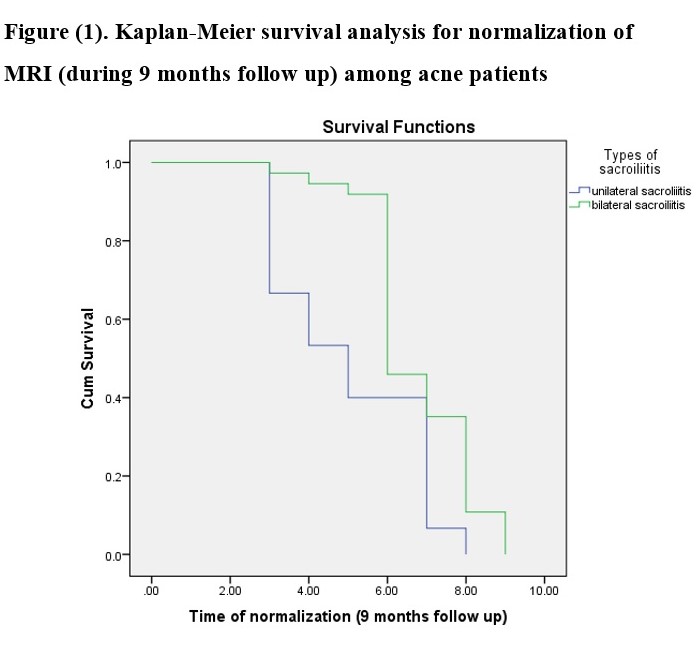
513 acne patients were enrolled, 123 (23.9%) developed IBP, and 88 (17.1%) developed arthralgia and arthritis .The mean onset of IBP was (2.1±0.85) months, with mean baseline pain score of (4.34±3.09). MRI proven sacroiliitis was found in (0.13%) of total number of acne patients, and (42.27%) of symptomatic patients, baseline CRP was (32.05±17.23 mg/L) and (3.4±2.7 mg/L) after being symptomless. 51.9% of the symptomatic patients had fulfilled the ASAS criteria for axial SpA, 97.6% of patients were treated with NSAID, however 2.4% were treated with anti TNF biologic. all cases normalized within 9 months, the mean time of normalization was (6.27±1.7) months. There was significant positive correlation for MRI scores, with pain, ASAS scores, baseline CRP. Unilateral sacroiliitis patients had significant rapid improvement than bilateral sacroiliitis (P<0.05).
Conclusion: Isotretinoin induced SpA is quite common side effect .Early rheumatologic assessment, and intervention is recommended. MRI is the modality of choice in early detection, and follow up of isotretinoin induced sacroiliitis.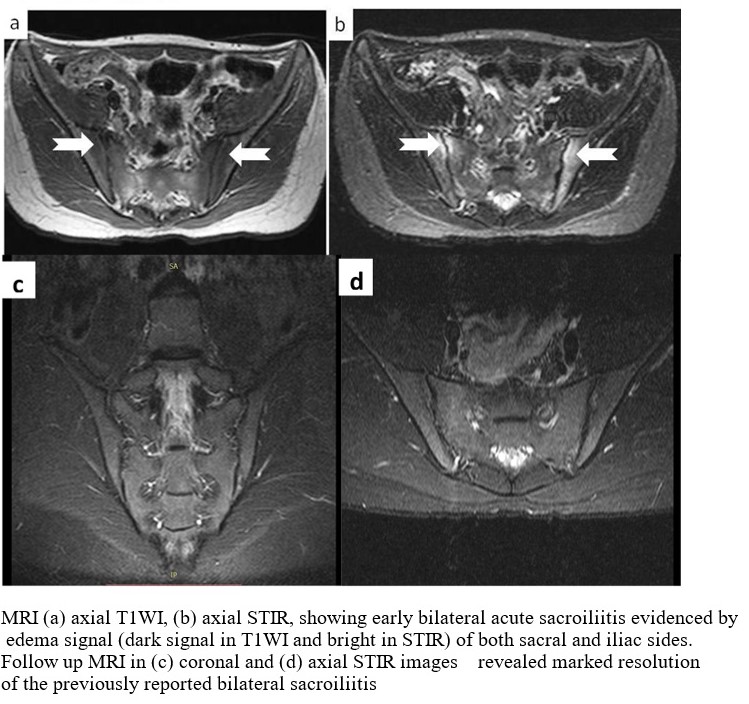
To cite this abstract in AMA style:
Elnady B, Desouky D, Elkhouly T, Dawoud N, Kewan H. Isotretinoin Induced Seronegative Spondyloarthropathy: Magnetic Resonance Imaging As Diagnostic and Prognostic Biomarker [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/isotretinoin-induced-seronegative-spondyloarthropathy-magnetic-resonance-imaging-as-diagnostic-and-prognostic-biomarker/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/isotretinoin-induced-seronegative-spondyloarthropathy-magnetic-resonance-imaging-as-diagnostic-and-prognostic-biomarker/
