Session Information
Date: Sunday, November 10, 2019
Title: Patient Outcomes, Preferences, & Attitudes Poster I: Patient Reported Outcomes
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) is accompanied by a high prevalence cardiovascular (CV) comorbidity. This comorbidity has been associated with worse therapeutic results as well as worse quality of life. We aimed to evaluate if the presence of this CV comorbidity could be associated with a greater impact of PsA on patients´ lives according to the Psoriatic Arthritis Impact of Disease (PsAID) questionnaire.
Methods: Post hoc analysis of a multicentre cross-sectional study that included 223 patients with PsA according to CASPAR criteria and under systemic treatment. The impact of the disease was assessed by the PsAID questionnaire. The impact of disease was evaluated by the PsAID, a questionnaire recently developed by the EULAR that reflects the impact of PsA from the patient’s perspective. It is comprised of 12 physical and psychological domains. Each domain is rated from 0 to 10 with a different weighting. The total score is divided by 20. The final score has a range from 0 (best status) to 10 (worst status) with a cut-off of 4. A PsAID value less than four has been defined as a patient-acceptable symptom state (PASS). A descriptive statistical analysis of all the variables was performed, including central tendency and dispersion measures for continuous variables, as well as absolute and relative frequencies for categorical variables. Student’s t-test, the Mann-Whitney U test, and the Kruskall-Wallis H-test were used to compare quantitative variables, and Pearson’s chi-square test or Fisher’s exact tests were used for qualitative variables. Concordance between different PsA outcomes was assessed using Cohen’s κappa (k) and was considered as follows: < 0.20 = poor, 0.21–0.40 = fair, 0.41–0.60 = moderate, 0.61–0.80 = good, and 0.81–1.00 = very good. The tests were two-tailed with a significance level of 5%. The data was analysed using SPSS V19.0 statistical software.
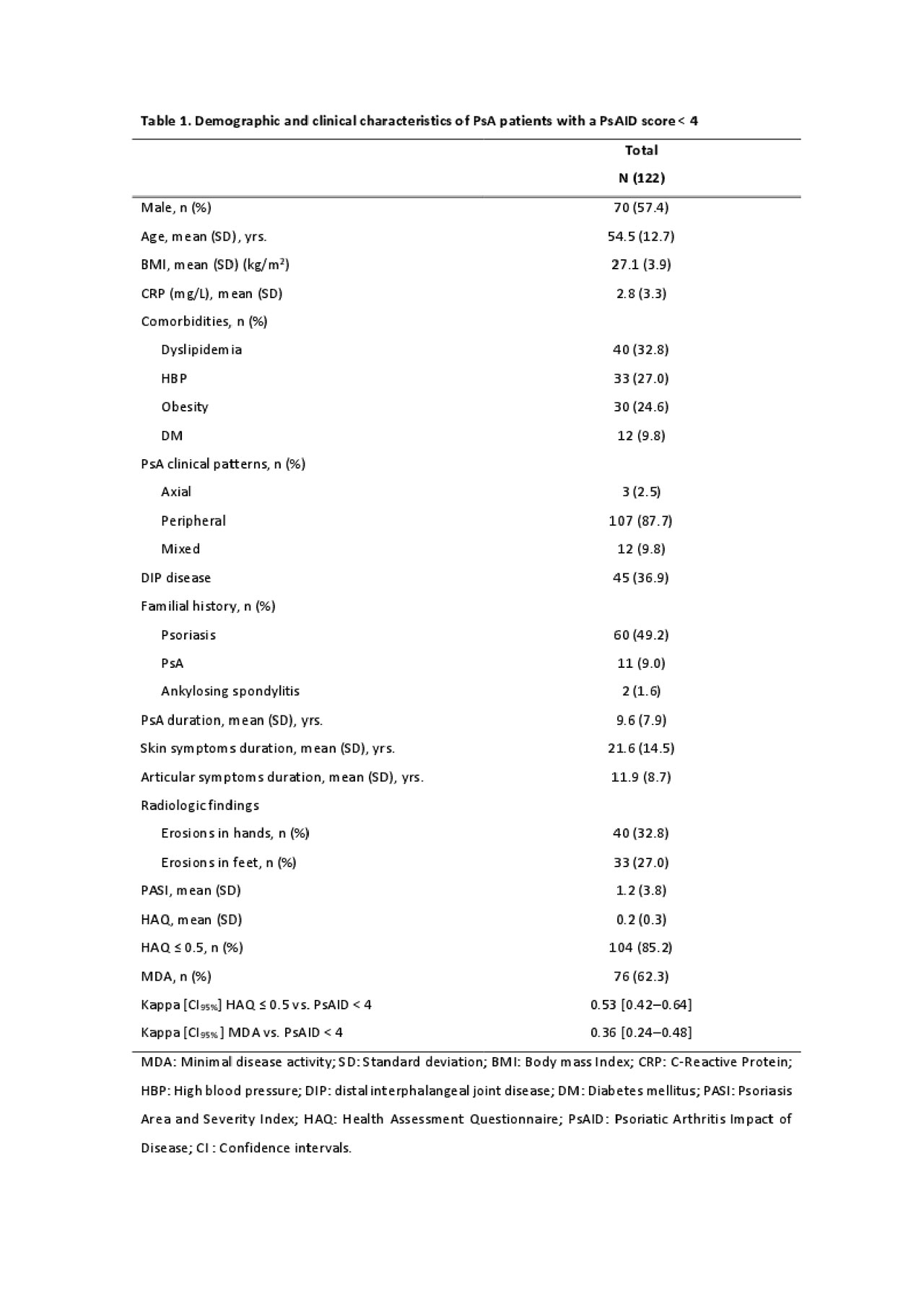
Results: Out of the 223 patients included in this analysis, 122 (54.7%) were in PASS status. The main characteristics of this subpopulation are shown in Table 1. There were more smokers among patients who did not achieve the PASS (25% vs. 13%, p= 0.08). However, there were more obese among those who did reach a PASS (24.6% vs. 15.8%, p= 0.108). No differences were found in the distribution of other CVRF between patients with and without PASS. Among PASS patients there was a significantly higher frequency of coronary heart disease (6.6%) than in non-PASS patients (1%), p = 0.035. The number of CV risk factors did not differ between the two groups.
Conclusion: In this multicentre study, we found no association between CV risk factors and the achievement of a PASS status in patients with PsA under systemic therapy. All in all, patients with PsA should be encouraged to maintain healthy lifestyle habits.
To cite this abstract in AMA style:
Queiro R, Pardo E, Charca L, Alonso S, Arboleya L, Alperi-López M. Is There Any Relationship Between Cardiovascular Comorbidity and a Patient-Acceptable Symptom State in Psoriatic Arthritis? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/is-there-any-relationship-between-cardiovascular-comorbidity-and-a-patient-acceptable-symptom-state-in-psoriatic-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-there-any-relationship-between-cardiovascular-comorbidity-and-a-patient-acceptable-symptom-state-in-psoriatic-arthritis/