Session Information
Date: Monday, October 22, 2018
Title: Spondyloarthritis Including Psoriatic Arthritis – Clinical Poster II: Clinical/Epidemiology Studies
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: A positive family history (PFH) of spondyloarthritis (SpA), in particular a PFH of ankylosing spondylitis (AS) or acute anterior uveitis (AAU), can be used to identify HLA-B27 carriership in chronic back pain patients1. It is unknown if a PFH contributes to diagnosing axial spondyloarthritis (axSpA) once HLA-B27 status is known.
Methods: Baseline data of patients suspected of axSpA in the ASAS, DESIR, and SPACE cohorts were analysed. Logistic regression analyses were performed with HLA-B27 status and PFH according to the ASAS definition (ASAS-PFH) as determinants and clinical axSpA diagnosis as the outcome. Analyses were repeated with a PFH of AS or AAU.
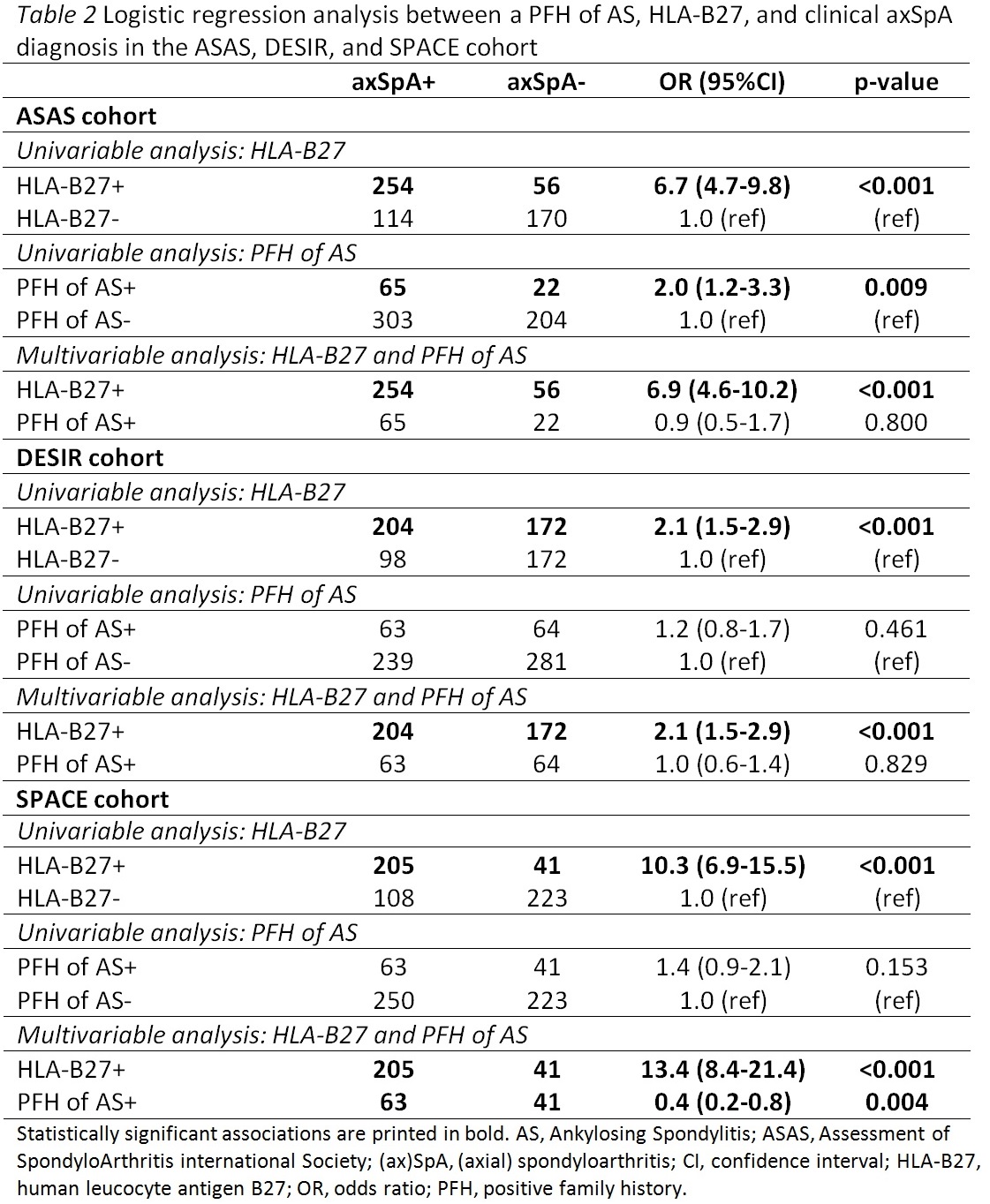
Results: In total, 1,964 patients suspected of axSpA were analysed (ASAS n=594, DESIR n=647, and SPACE n=577). Patients from the ASAS, DESIR, and SPACE cohorts, respectively had a mean (SD) symptom duration of 85.7 (108.4), 18.2 (10.5), and 13.3 (7.1) months; 46%, 47%, and 38% were male; 23%, 39%, and 38% had an ASAS PFH, 52%, 58%, and 43% were HLA-B27 positive, and 62%, 47%, and 54% were diagnosed with axSpA. In the univariable analysis, HLA-B27 status was significantly associated with an axSpA diagnosis in all three cohorts (Table 1). An ASAS-PFH and a PFH of AAU were univariately associated with an axSpA diagnosis in the SPACE cohort, but not in the ASAS and DESIR cohorts. A PFH of AS was associated with an axSpA diagnosis in the ASAS cohort, but not in the DESIR and SPACE cohorts. In the multivariable models, HLA-B27 was independently and positively associated with an axSpA diagnosis in each cohort but such an independent positive association was not found for an ASAS-PFH in any cohort (Table 1). Similarly, a PFH of AS did not have an independent positive association with an axSpA diagnosis in any cohort (Table 2). Similar results were found for PFH of AAU (ASAS cohort: HLA-B27 OR:6.9 (95%CI:4.7-10.1), ASAS PFH OR:0.4 (95%CI:0.08-1.8); DESIR cohort: HLA-B27 OR:2.1 (95%CI:1.5-2.9), ASAS PFH OR:1.1 (95%CI:0.5-2.3); SPACE cohort: HLA-B27 OR:10.7 (95%CI:7.0-16.3), ASAS PFH OR:0.8 (95%CI 0.3-1.8)).
Conclusion: A PFH did not contribute independently of HLA-B27 to a diagnosis of axSpA in axSpA suspected patients.
References: 1Ez-Zaitouni et al (2017), AR&T 2017;19(1):118.
To cite this abstract in AMA style:
van Lunteren M, van der Heijde D, Sepriano A, Berg I, Dougados M, Gossec L, Jacobsson L, Ramonda R, Rudwaleit M, Sieper J, Landewé RBM, van Gaalen F. Is a Positive Family History of Spondyloarthritis Relevant for Diagnosing Axial Spondyloarthritis Once HLA-B27 Status Is Known? Data from the ASAS, DESIR, and SPACE Cohorts [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/is-a-positive-family-history-of-spondyloarthritis-relevant-for-diagnosing-axial-spondyloarthritis-once-hla-b27-status-is-known-data-from-the-asas-desir-and-space-cohorts/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-a-positive-family-history-of-spondyloarthritis-relevant-for-diagnosing-axial-spondyloarthritis-once-hla-b27-status-is-known-data-from-the-asas-desir-and-space-cohorts/