Session Information
Date: Tuesday, November 12, 2019
Title: Pediatric Rheumatology – ePoster III: Systemic JIA, Fever, & Vasculitis
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Inactive disease is the stated goal of treatment in juvenile idiopathic arthritis (JIA) and is typically measured by a composite score that combines several different factors including provider and parent or patient assessments. Various definitions of inactive disease may identify different JIA populations because each score utilizes different components. We compared and contrasted the JIA patients who met various definitions for inactive disease.
Methods: We used the Childhood Arthritis & Rheumatology Research Alliance (CARRA) Registry of clinical data from >65 pediatric rheumatology clinics in the United States and Canada. Individuals with JIA with at least 12 months of observable time after enrollment and completion of the 1 year follow up visit were included. Individuals were excluded if they had incomplete inactive disease measures at the 1-year visit. Demographic and disease characteristics were reported at baseline and the 1-year visit to allow for at least 1 year of disease duration. The frequency and proportion of outcomes for all patients at 1-year follow up were reported regardless of disease duration. The Pearson correlation coefficient was calculated between physician global, patient global, active joint count, and pain at 1-year for all patients.
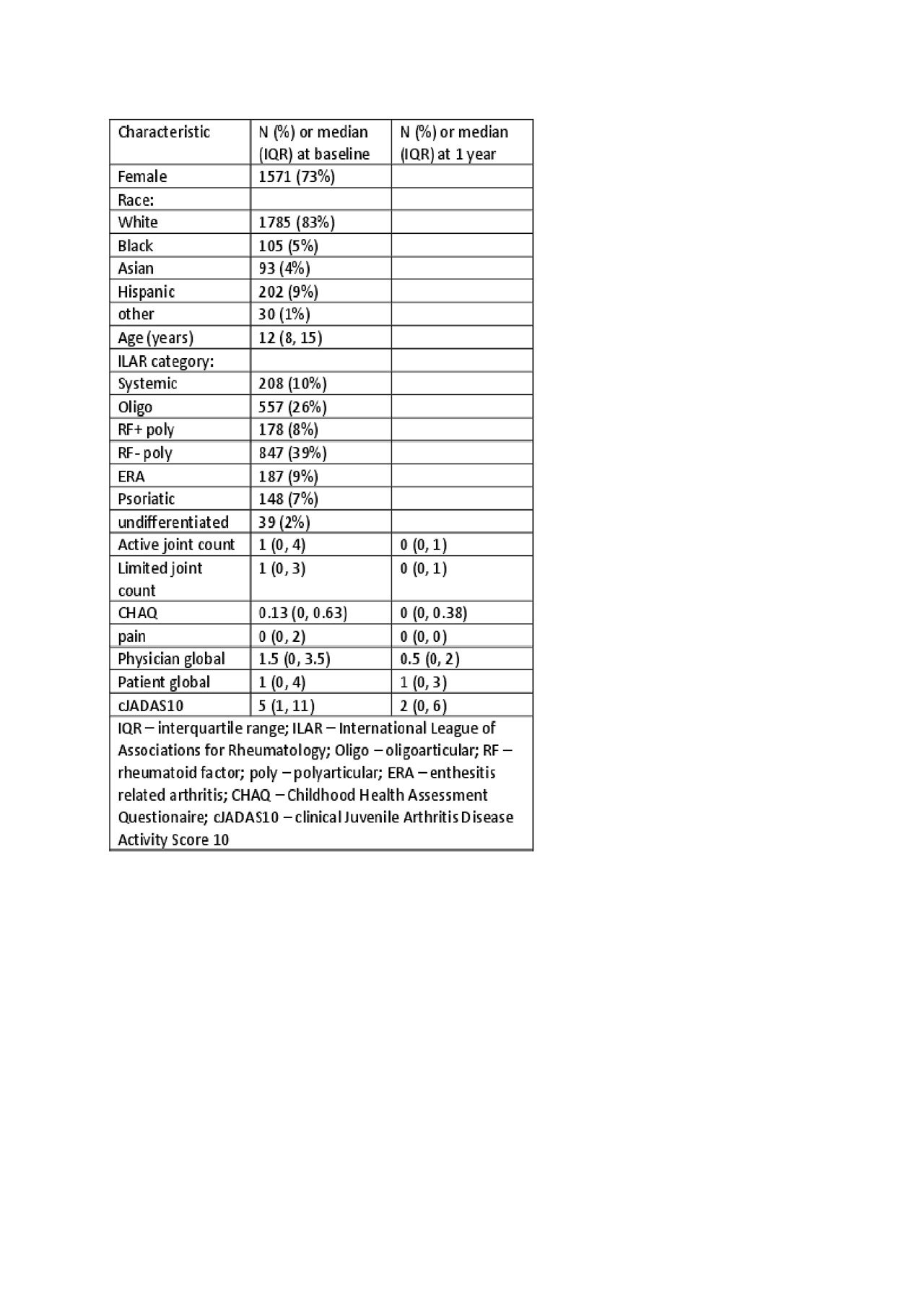
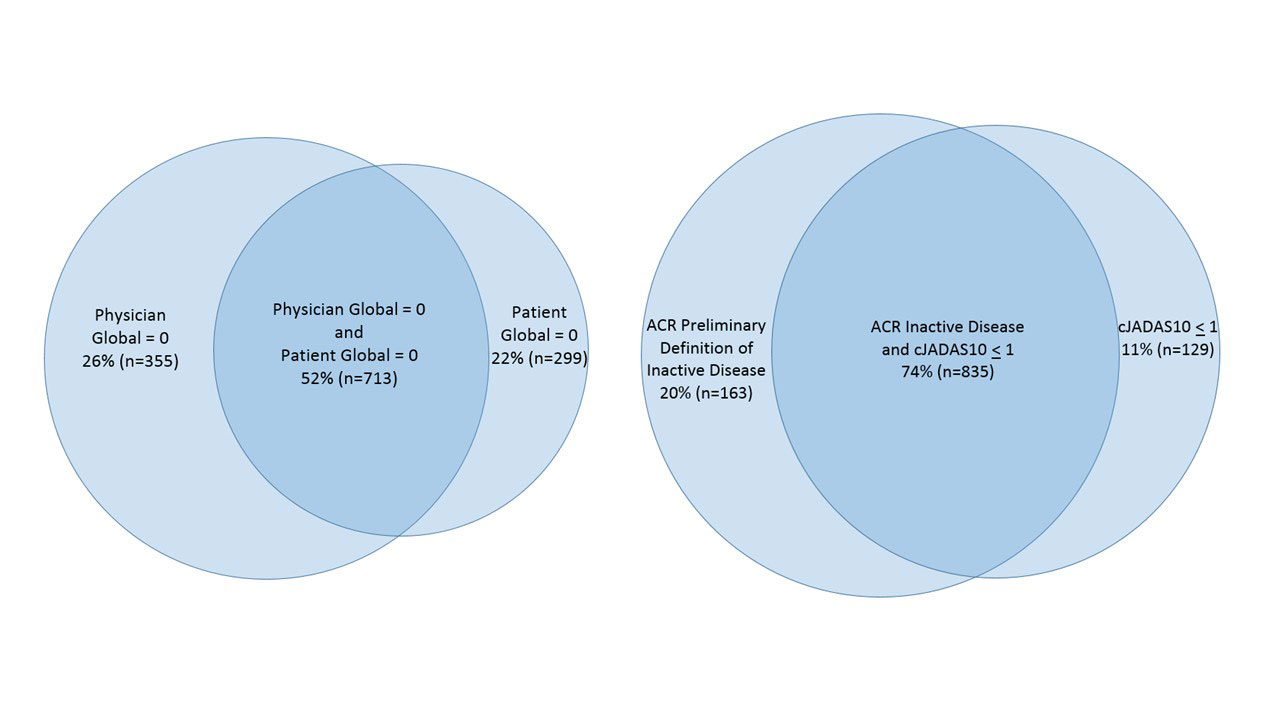
Results: There were 2164 JIA patients enrolled in the CARRA Registry with completion of 1-year follow up visit (Table 1). Of these 2164 individuals, 70% were treated with a conventional disease modifying anti-rheumatic drug (DMARD) between enrollment and 1-year follow up and 66% were treated with a biologic DMARD. Among all 2164 individuals at the 1-year visit, 1453 (67%) had no active joints, 1068 (49%) had a physician global of 0, 1012 (47%) had a patient global of 0, 998 (46%) met the American College of Rheumatology preliminary criteria for clinical inactive disease (ACR CID), and 964 (45%) had a clinical Juvenile Arthritis Disease Activity Score 10 (cJADAS10) < 1 (Figure 1). There was moderate correlation between physician global and active joint count (R=0.62, p< 0.001), patient global and pain score (R=0.48, p< 0.001), physician global and patient global (R=0.45, p< 0.001), patient global and active joint count (R=0.32, p< 0.001), and a weak correlation between physician global and pain score (R=0.24, p< 0.001).
Conclusion: In a multicenter cohort of JIA patients in North America, a large proportion of patients had inactive disease by single or composite measures after 1 year of observation in the Registry. There was significant overlap between patients who met ACR CID criteria and cJADAS10 < 1 which may indicate acceptable use of either composite measure for disease management in the clinical setting. Additional studies are needed to evaluate the reasons for discordance in inactive disease measures and to identify the clinical outcomes following achievement of inactive disease by different composite measures.
This study was performed with the support of the CARRA Registry Investigators.
To cite this abstract in AMA style:
Mannion M, Xie F, Beukelman T. Investigation of Inactive Disease Activity States Among JIA Patients in the CARRA Registry [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/investigation-of-inactive-disease-activity-states-among-jia-patients-in-the-carra-registry/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/investigation-of-inactive-disease-activity-states-among-jia-patients-in-the-carra-registry/