Session Information
Date: Sunday, November 17, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Giant cell arteritis is being increasingly recognized to occur in intracranial vessels. The clinical significance of intracranial GCA (ICGCA) is unknown; previous cases have suggested changes in the cerebral vasculature are associated with stroke. We identified all reported cases of ICGCA to describe common presentations, investigations, treatments, and outcomes reported.
Methods: We conducted a systematic review using MEDLINE, Embase and Pubmed to identify studies that reported cases of ICGCA. The study was registered on a systematic review database (PROSPERO 42023412373). We defined intracranial involvement as any vessel cranial to the dura mater that was confirmed by either histopathology or imaging. Abstract screening, full text screening, and data abstraction were performed in duplicate with any disagreements adjudicated by a third investigator. Data was summarized using descriptive statistics.
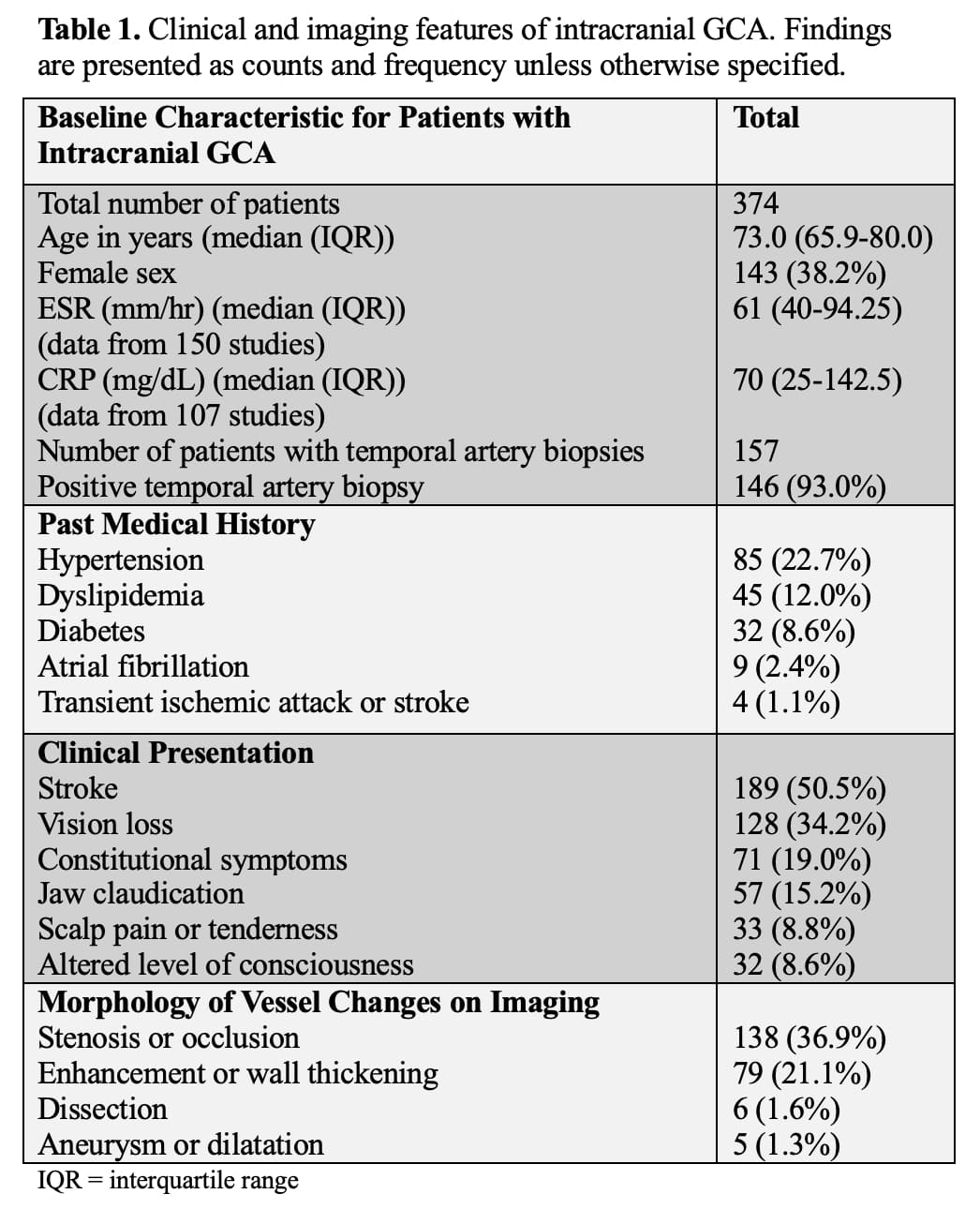
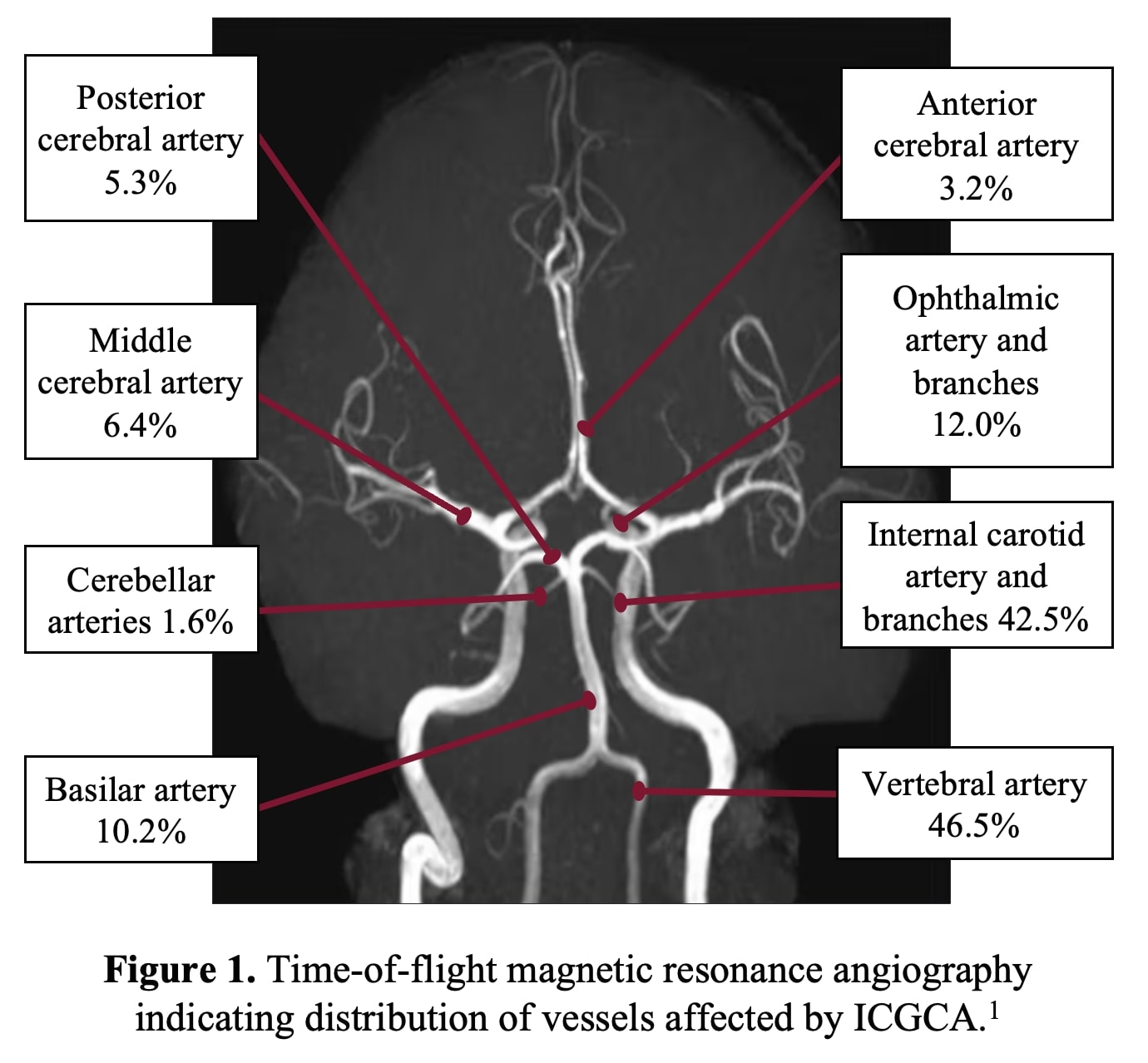
Results: A total of 1554 studies underwent title and abstract screening, 424 underwent full text screening and 114 studies were included. These studies included 374 patients with ICGCA. The median age was 73.0 (interquartile range (IQR) 65.9-80.0) and 143 (38.2%) patients were female (Table 1). Presentations of ICGCA included 189 (50.5%) cases with stroke, 128 (34.2%) presented with vision loss, and 71 (19.0%) presented with constitutional symptoms. The most common vessels involved were 159 (42.5%) internal carotid, 174 (46.5%) vertebrobasilar, and 49 (13.1%) ophthalmic arteries (Figure 1). Across individuals with stroke, 113 (59.8%) had cerebral strokes, 44 (23.3%) had brainstem strokes, and 35 (18.5%) had cerebellar strokes. Treatment was reported in 193 individuals. Glucocorticoids were administered to 185 (94.3%) of patients; cyclophosphamide was administered to 45 (23.3%), 33 (17.1%) methotrexate, and 30 (15.5%) tocilizumab. Of the 144 patients with reported follow-up outcomes, relapse (one or more) occurred in 34 (24.0%), 18 (12.5%) had a recurrent stroke, and 63 (44.0%) died. Of the individuals with disease relapse, 28 (82.4%) had relapse of their intracranial disease.
Conclusion: These findings suggest that intracranial vasculitis in GCA is more frequent than previously thought and is associated with increased morbidity and mortality. Optimal therapy for ICGCA is unknown. Structured prospective evaluation is needed to better understand the burden of ICGCA, outcomes, and effective approaches to management.
[1.] Micheau A, Hoa D. doi:10.37019/e-anatomy/520281
To cite this abstract in AMA style:
Patel S, Okaj I, Scott J, Atwal S, Stark C, Tahir R, Khalidi N, Junek M. Intracranial Giant Cell Arteritis: A Comprehensive Systematic Review [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/intracranial-giant-cell-arteritis-a-comprehensive-systematic-review/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/intracranial-giant-cell-arteritis-a-comprehensive-systematic-review/