Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The transition from pediatric to adult care is a vulnerable period, in which poor health outcomes are reported amongst youth transferring to adult care. We sought to improve the efficiency of the referral process and established dedicated appointment slots for patients transferring from pediatric to adult care in our large safety-net hospital system.
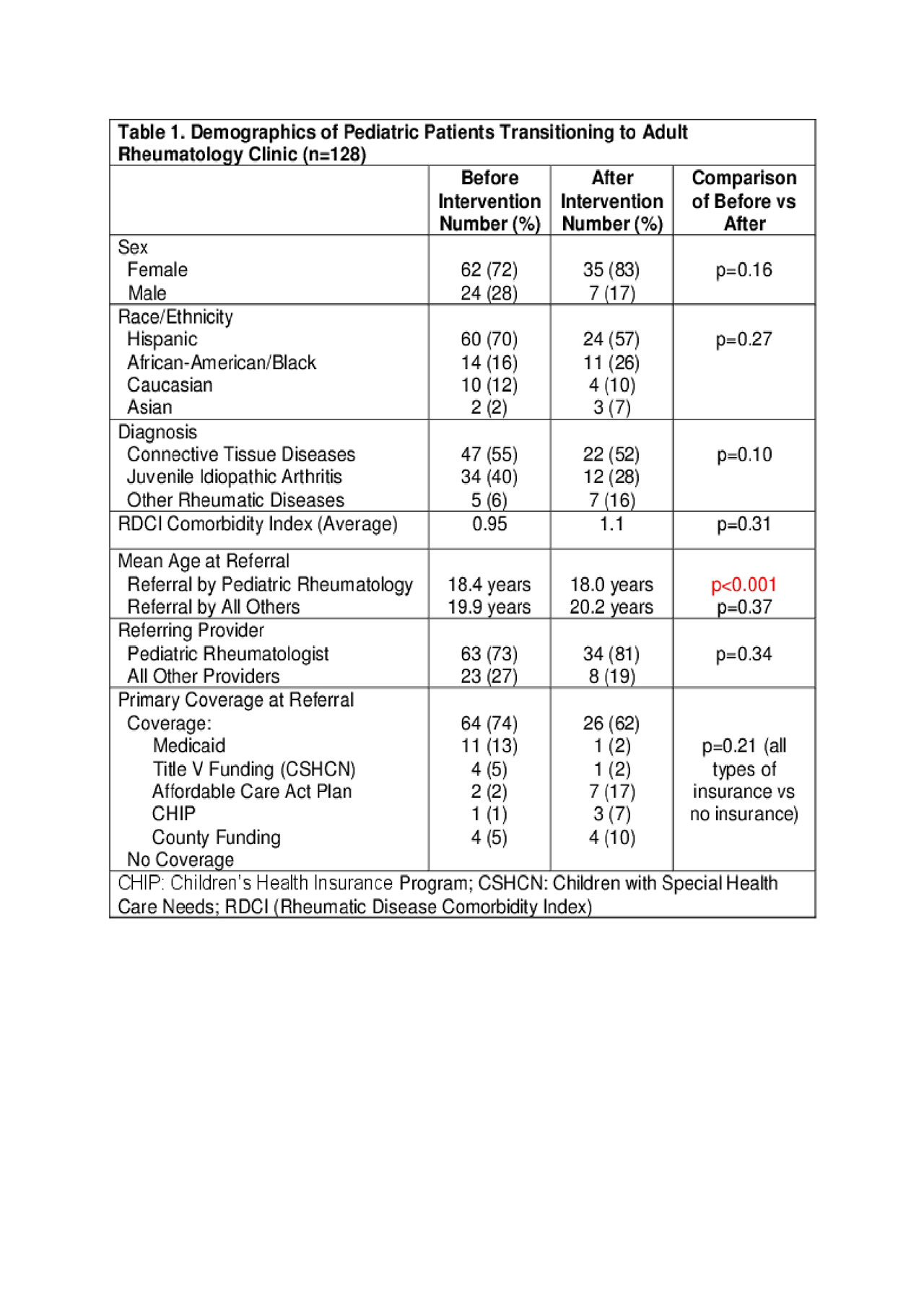
Methods: A chart review was conducted from eight-six pediatric patients between ages 17 and 21 transitioning to a safety-net adult rheumatology clinic between March 2014 and February 2018 (pre-intervention) and 42 patients from March 2018 to April 2019 (post-intervention). Independent variables included demographic information, diagnoses, referring physician type (pediatric rheumatologist or other), communication between pediatric and adult physicians, and lapse in medical coverage of greater than 30 days between final pediatric and first adult visit. The relationship between these variables and outcomes of interest was analyzed including time between referral and first appointment, time between final pediatric and first adult visit, healthcare utilization between referral and first adult visit including hospitalizations and ED visits, and self-reported medication non-adherence at first visit. Comparisons were made using Chi-square and Mann-Whitney U tests.
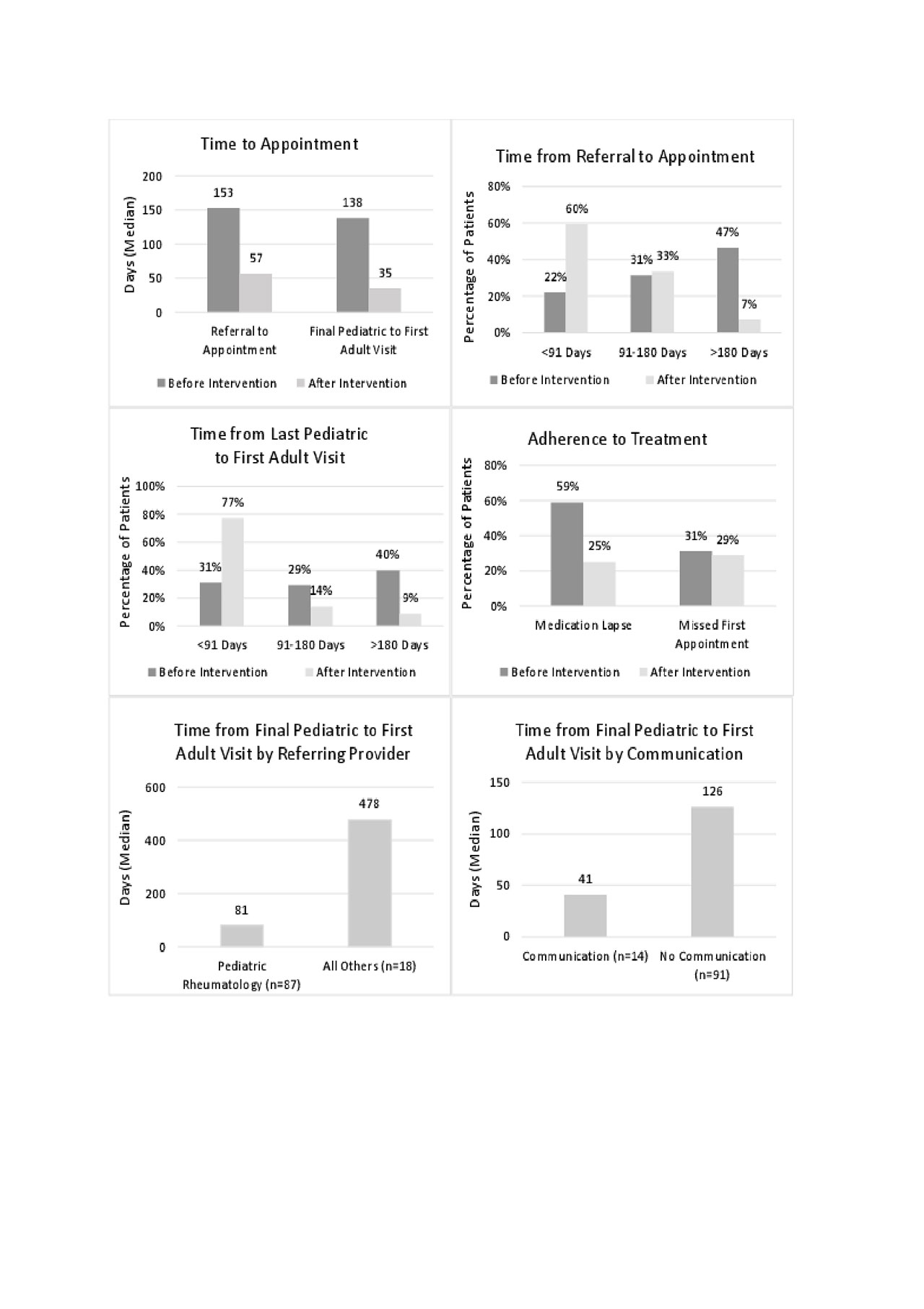
Results: Pre-intervention, the interval between referral and appointment with adult rheumatology was a median of 158 days, which declined to a median of 35 days post intervention (average 80 days). Interval between final pediatric to first adult visit also declined from a median of 153 days to 57 days post-intervention (p< 0.01). As the intervention was based on identifying referrals from the main pediatric rheumatology clinics in the area, those who were not referred to adult care by pediatric rheumatologists continued to have prolonged time to first visit. Hospitalizations and emergency department visits during the interim period between pediatric and adult visits declined significantly, as did self-reported medication non-adherence at first adult visit (from 59% to 25%). Initial missed appointment with adult rheumatology remained unchanged by the intervention.
Conclusion: Youth transitioning into adult rheumatology experience significant delays to first adult rheumatology visit, but dedicated appointment slots and improving the referral process were effective in reducing time to first adult appointment, decreasing health care utilization during the transfer period, and decreasing self-reported medication non-adherence at first visit. It remains important that pediatric rheumatologists ensure they refer all appropriately-aged patients to adult care.
To cite this abstract in AMA style:
Bitencourt N, Makris U, Bermas B, Wright T, Solow E. Interventions to Improve Time to Appointment and Outcome Variables in the Pediatric to Adult Transition of Care in Rheumatology [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/interventions-to-improve-time-to-appointment-and-outcome-variables-in-the-pediatric-to-adult-transition-of-care-in-rheumatology/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/interventions-to-improve-time-to-appointment-and-outcome-variables-in-the-pediatric-to-adult-transition-of-care-in-rheumatology/