Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Prior data suggest sociodemographic and regional variability in various indicators of quality of end-stage renal disease (ESRD) care, both overall and in the SLE population, but, to our knowledge, no study has addressed the placement of a permanent vascular access prior to the start of hemodialysis in patients with ESRD secondary to lupus nephritis (LN-ESRD). We aimed to describe permanent vascular access placement among hemodialysis patients with LN-ESRD and to examine whether this placement differs by sociodemographic factors and across the 18 U.S. ESRD Networks, which are Centers for Medicare & Medicaid Services-defined regions that implement ESRD quality-of-care initiatives.
Methods: Among 5562 incident U.S. hemodialysis patients with LN-ESRD initiating treatment 7/05-9/11, we estimated the associations between permanent access placement (arteriovenous fistula or graft used or in place on first dialysis, vs. temporary catheter only) and race/ethnicity, insurance at the start of ESRD, and ESRD Network using national surveillance data (United States Renal Data System). Logistic regression models were used to estimate odds ratios (ORs) and confidence intervals (CIs), with adjustment for potential demographic (age, sex, race/ethnicity, insurance) and clinical (BMI, hypertension, cardiovascular disease) confounders.
Results: Fewer than one-quarter (24.4%) of incident hemodialysis patients with LN-ESRD patients had a permanent vascular access placed at start of dialysis, compared to 36.0% of other ESRD patients. Hispanic LN-ESRD patients were less likely than their white counterparts to have a permanent vascular access (20.5% vs. 28.2%), but the association was not statistically significant after adjustment (OR=0.85; 95% CI, 0.69-1.05). Placement did not differ in black vs. white LN-ESRD hemodialysis patients. After adjustment, private, Medicaid, and other insurance were associated with equivalent likelihood of permanent vascular access, but having no insurance was associated with 38% lower likelihood of permanent vascular access among LN-ESRD patients (OR=0.62; 95% CI, 0.49-0.79). There was substantial, statistically significant Network-level variation in likelihood of permanent vascular access, with adjusted probabilities of permanent vascular access used or in place at first dialysis ranging nearly 2-fold, from 0.17 (Network 10, Illinois) to 0.33 (Network 16, Northwest).
Conclusion: The vast majority of LN-ESRD patients on hemodialysis are not initiating treatment with a permanent vascular access. LN-ESRD patients who are Hispanic or uninsured or who live in the Midwest or Southern California at the start of ESRD are less likely to have permanent vascular access. Targeted interventions to increase permanent vascular access among SLE patients with ESRD are warranted to prevent potential morbidity and mortality associated with temporary catheters.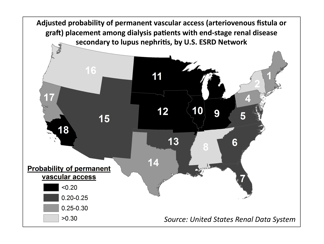
Disclosure:
L. Plantinga,
None;
C. M. Drenkard,
None;
R. Patzer,
None;
W. McClellan,
None;
S. Pastan,
None;
S. S. Lim,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/insurance-status-and-u-s-region-associated-with-placement-of-permanent-vascular-access-in-dialysis-patients-with-end-stage-renal-disease-secondary-to-lupus-nephritis/
