Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Current RA guidelines recommend treating to a target of remission or low disease activity (RM/LDA) state. In a prior quality improvement (QI) project, our practice increased documentation of Rapid3 in provider notes to 92%. This QI project was developed to improve the percentage of our RA patients in RM/LDA, as measured by Rapid3. We also aimed to understand providers’ attitudes and use of the Rapid3 in practice.
Methods:
We reviewed charts of established (>1 prior visit) RA patients over an 8-month period to assess use of Rapid3 in decision-making. We recorded Rapid3 presence and value, relevant co-morbidities (FM, OA and mood-disorders) and whether a change in therapy was made. Using Plan-Do-Study-Act (PDSA) methodology, we introduced the following interventions to improve utilization: education through Grand Rounds, modification of electronic medical record templates and reminder emails to providers. Charts were analyzed at baseline, between interventions and at the conclusion of all interventions. We surveyed providers at baseline and at project completion regarding habits and attitudes towards Rapid3 in clinical practice.
Results:
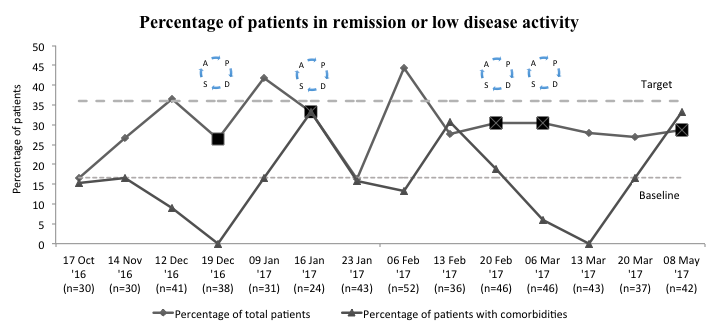
Of 539 patient encounters with established RA, Rapid3 was documented in 501 encounters (93%). About 55% had at least 1 relevant co-morbid condition (182 patients with OA, 79 with FM, 74 with mood disorders); 295 had 1 co-morbidity, 34 had 2 co-morbidities and 6 had 3 co-morbidities. At baseline 38/139 (27%) were in RM/LDA. Our interventions resulted in 123/362 (34%) patients in RM/LDA (Figure 1). At almost every time point, percent of patients achieving RM/LDA was highest in patients with RA and no co-morbidities (Figure 1). Our survey of 18 providers found only 17% felt Rapid3 accurately reflected RA disease activity most of the time; 78% agreed Rapid3 changed their clinical management <10% of the time. Providers indicated the greatest challenges in using of Rapid3 were “score does not represent RA activity” and “other co-morbidities.”
Conclusion:
We sustained documentation rates of Rapid3 above 90%. The percent of patients in RM/LDA slightly improved, but this intervention was limited by short duration. We found very low provider confidence that the Rapid3 reflected RA activity, and it was infrequently used as a treatment target. The presence of any selected co-morbidities demonstrated a lower likelihood of achieving RM/LDA by Rapid3; FM and mood disorder had the greatest impact. Rapid3 may be most useful in patients without these co-morbidities. In the future, a “correction factor” for co-morbidities in scoring of Rapid3 may improve accuracy and provider use.
To cite this abstract in AMA style:
Jayasundara M, Jessee R, Weiner J, Haroun T, Giattino S, Kapila A, Hall J, Carnago L, Criscione-Schreiber L. Insights from Treating to Target in Rheumatoid Arthritis at an Academic Medical Center [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/insights-from-treating-to-target-in-rheumatoid-arthritis-at-an-academic-medical-center/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/insights-from-treating-to-target-in-rheumatoid-arthritis-at-an-academic-medical-center/