Session Information
Date: Monday, November 6, 2017
Title: Osteoporosis and Metabolic Bone Disease – Clinical Aspects and Pathogenesis Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammatory bowel diseases (IBD), such as Crohn disease (CD) and ulcerative colitis (UC), are associated with a decreased bone mineral density caused by chronic inflammation and corticosteroid use. However, the increase of fracture risk is unknown and data are contradictory across studies.
The aim of our study was to assess the risks of fracture and presence of low bone mineral density (BMD) in patients with IBD compared to the general population.
Methods : A systematic search of literature up to 1st February 2017 was conducted using databases including: MEDLINE (via PUBMED), EMBASE, the Cochrane library and abstracts from the ACR, ASBMR and EULAR congresses 2014-2016. Prospective and retrospective cohort studies were included if they reported the incidence of fractures and/or the measure of BMD by dual energy X-ray absorptiometry (DXA) (expressed in g/cm2) in IBD patients in comparison with healthy controls. Data was extracted by two independent investigators. Meta-analysis was performed to assess odds-ratios (OR) for each outcome using the inverse variance approach to estimate pooled OR with their 95% confidence interval. Heterogeneity was assessed according to Cochran Q-test and I2 values. Calculations were made with the Cochrane RevMan 5.3 software. P-values less than 0.05 were considered significant.
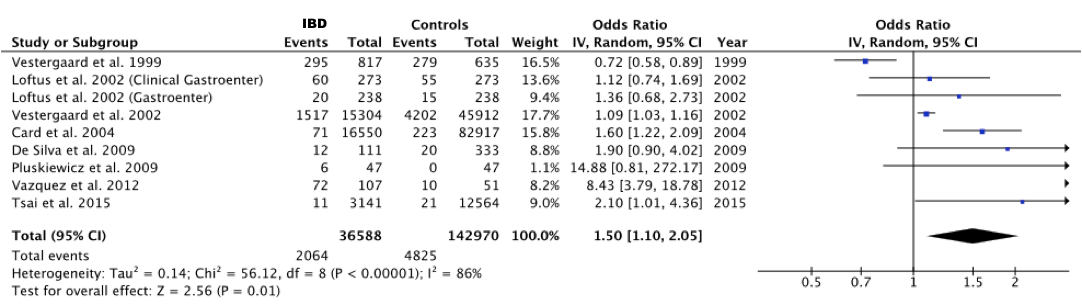
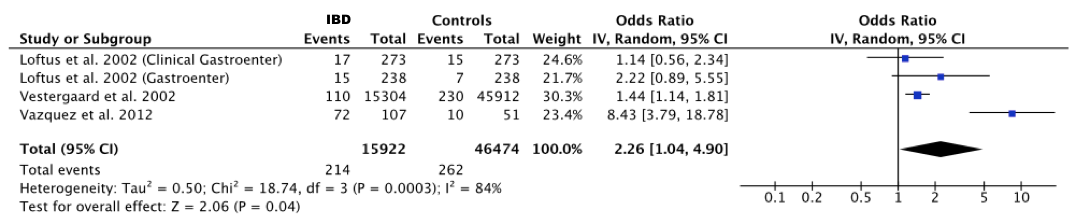
Results : The literature search identified 1165 articles and no congress abstract; a manual search did not retrieve any additional article. Finally, 25 studies met the inclusion criteria. Nine of them reported 2065 fracture events among 42,615 IBD patients and 4825 fracture events among 203,240 healthy controls. Global risk of fracture was increased in IBD patients compared with controls with a pooled OR of 1.50 (95% CI 1.10-2.05; p=0.01, I2=86%). The pooled OR of vertebral fracture was 2.26 (95% CI 1.04-4.90; p < 0.001, I2=84%). Fracture risk was not significantly increased for any other site (arm, hip, wrist). The analysis of 17 studies concerning BMD showed a significant decrease of BMD and Z-score at three sites. At femoral neck, mean difference (MD) of BMD was -0.05 (95% CI -0.08 to -0.02; p=0.001, I2=60%) and MD of Z-score -0.48 (95% CI -0.64 to -0.33; p<0.00001, I2=0%). These values were respectively -0.08 (95% CI -0.11 to -0.05, p<0.00001, I2=46%) and -1.01 (95% CI -1.52 to -0.50; p=0.07, I2=69%) at total femur, and -0.06 (95% CI -0.10 to -0.03, p=0.0003, I2=87%) and -0.51(95% CI -0.68 to -0.34; p<0.0001, I2=54%) at lumbar spine.
Conclusion: IBD patients have an increased risk of fractures, especially in the spine, and a decrease of BMD at all sites, suggesting the need for regular follow-up and preventing measures.
To cite this abstract in AMA style:
Szafors P, Barnetche T, Lukas C, Morel J, Gaujoux-Viala C, Combe B, Che H. Inflammatory Bowel Diseases and the Risks of Fracture and Low Mineral Density: Review of the Literature and Meta-Analysis of Observational Cohorts [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/inflammatory-bowel-diseases-and-the-risks-of-fracture-and-low-mineral-density-review-of-the-literature-and-meta-analysis-of-observational-cohorts/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inflammatory-bowel-diseases-and-the-risks-of-fracture-and-low-mineral-density-review-of-the-literature-and-meta-analysis-of-observational-cohorts/