Session Information
Date: Sunday, October 21, 2018
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Arthroplasty requirements among patients with psoriatic arthritis (PsA) are not well known. This information is of importance to clinical and policy stakeholders for health system planning, and may serve as a surrogate for estimating the efficacy of disease-modifying therapy. Moreover, arthroplasty rates may be used as a proxy measure of how advanced medical therapy has contributed to the prevention of advanced-stage disease, as has been done previously for rheumatoid arthritis.
Methods: We utilized The Health Improvement Network (THIN), a large general practice medical records database in the United Kingdom to assess rates of first primary total arthroplasty among patients with PsA and the general population between the years 1995 and 2010. Linear regression was used to estimate arthroplasty rates for the two cohorts over the study period, and Poisson regression was used to determine incidence rate ratios (IRRs) between the PsA and general population cohorts, adjusted for age and sex. Chi-square tests were used to compare incidence rates across years between the two cohorts.
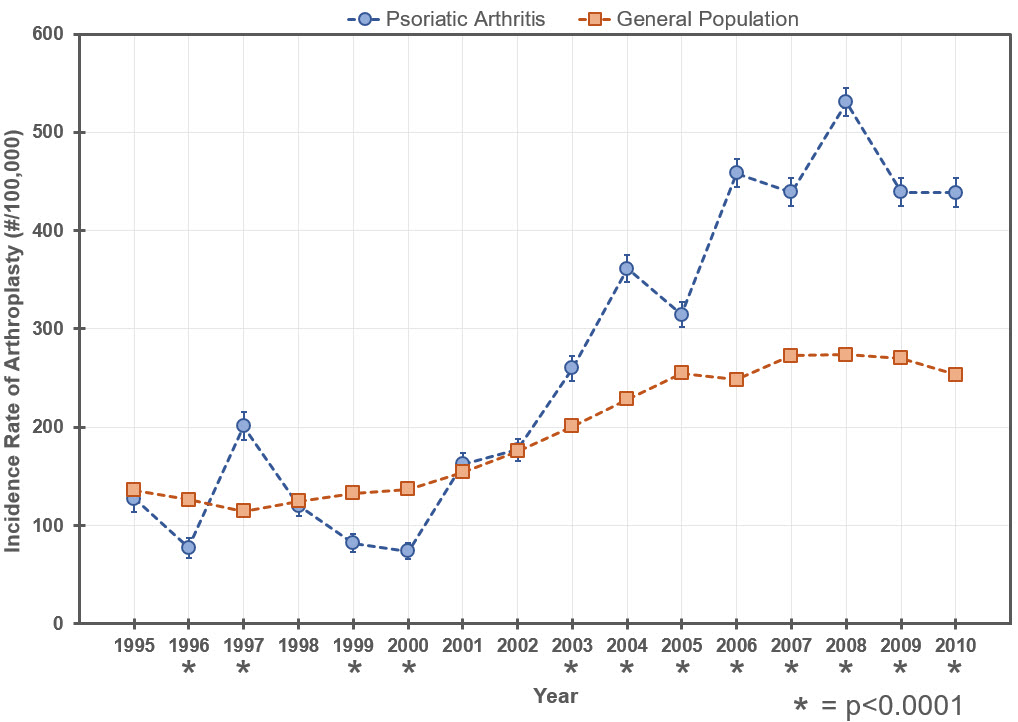
Results: We identified 5,619 patients with incident PsA and 5,090,814 eligible patients from the general population between 1995 and 2010. In total, 187 first primary total arthroplasties were documented in patients with PsA, and 80,165 first primary total arthroplasties were documented in the general population. A trend of increased arthroplasty rates were observed for both the PsA (R2=0.809, p<0.0001) and general population (R2=0.890, p<0.0001) cohorts over the study period. After adjustment for age and sex, PsA patients had a first arthroplasty incidence rate twice that of the general population (IRR=2.01, 95%CI 1.73-2.34, p<0.0001), notably beyond year 2003 when biologic therapies were introduced (Fig. 1).
Conclusion: Both general population and PsA patients have experienced increased rates of first arthroplasty from 1995 to 2010, although the overall incidence rate was significantly higher for those with PsA. There are a number of possibilities that could explain this finding such as patients living longer with PsA, or new biologic therapies making PsA patients better surgical candidates. Further research exploring these possibilities will be needed in the coming years.
Figure 1
Figure 1. Incidence rates (with 95% Confidence intervals) of first arthroplasty are shown for both the psoriatic arthritis cohort (blue circles) and the general population cohort (orange squares). The incidence rate of arthroplasty has increased for both groups from 1995 to 2010. *indicates significant difference in incidence rates by Chi-square test. Evaluation of the overall incidence rate ratio (IRR) revealed PsA patients had an incidence rate of first arthroplasty twice that of the general population (IRR 2.01, 95%CI 1.73-2.34, p<0.0001).
To cite this abstract in AMA style:
Lewinson R, Vallerand I, LaMothe J, Parsons L, Frolkis A, Lowerison M, Patten S, Barnabe C. Increasing Rates of Arthroplasty for Psoriatic Arthritis in the United Kingdom between 1995 and 2010 [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/increasing-rates-of-arthroplasty-for-psoriatic-arthritis-in-the-united-kingdom-between-1995-and-2010/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increasing-rates-of-arthroplasty-for-psoriatic-arthritis-in-the-united-kingdom-between-1995-and-2010/