Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose:
Low body mass index (BMI) is a known risk factor for loss of bone mineral density (BMD). It is a part of the FRAX ™ 10-year fracture risk stratification tool developed by the World Health Organisation. It is also known that weight loss through dieting decreases BMD, whilst weight loss through exercise preserves it. The effects of fat-mass and change in fat-mass have not been examined extensively. This could have implications for health advice given to those at significant risk of fragility fractures. This study aimed to identify factors influencing change in bone density related to fat-mass and any confounders.
Methods:
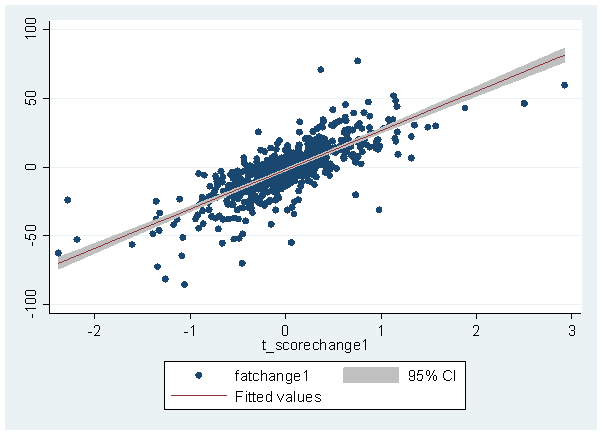
Data were analysed from patients having dual-energy X-ray absorptiometry (DXA) assessment between 2007 and 2010. Patients were included if they had multiple scans which included measurements of lean mass and fat mass. Our scanners limited these to scans of the AP spine. Linear regression was performed to determine the relationship between changes in fat mass and BMD. A backwards stepwise linear regression model was fitted with inclusion of confounders including: sex, risk factors, previous fractures, baseline BMI and age at menopause.
Results:
23,239 patients were included in the study, of which 702 met our inclusion criteria. This included 93 males (13%) and 609 females (87%). Mean age at first scan in the whole cohort was 64.5 years (SD11.2). The mean interval between scans was 3.0 years (SD 0.89). Step-wise linear regression identified a positive correlation between increasing fat-mass and t-score per unit time between scans (coefficient 28.4, p<0.01 95%CI 26.6-30.1). Controlling for the above factors didn't alter the results. We identified previous pelvic and femur fractures (p<0.05) and history of inflammatory diseases (p<0.05) as independent risk factors influencing bone density related to fat mass. This relationship was true for patients that were underweight (BMI <18.5), normal weight (BMI 18.5-25), and overweight patients (BMI >25).
Conclusion:
Increasing fat mass between DEXA scans is associated with an increase in t-scores. Other factors associated with increasing fat-mass include previous pelvic and femur fractures, as well as history of inflammatory disease. However, excessive fat-mass is associated with increased cardiovascular (CVD) and metabolic disease states. Increasing fat-mass is therefore not viable for all patients. Those at particular risk of fragility fractures and not CVD, e.g. BMI<18.5, may be able to improve their long-term risk by gaining weight.
Disclosure:
W. Hedges,
None;
M. Bukhari,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increasing-fat-mass-may-reverse-bone-loss-as-detected-by-dxa-scan/