Background/Purpose We have seen remarkable achievements in disease control (DAS28) in rheumatoid arthritis in the past decade. They were, however, not accompanied to the same degree by improvements in patient reported outcomes. To evaluate whether the relationship between patient global health and physician assessment of disease activity, both measured on numerical rating scales 0-10, has changed in the last decade and if these changes differ between diagnoses or depend on sex, age, disease duration or education.
Methods Patients recorded in the National Database of the German Collaborative Arthritis Centres between 2000 and 2012 for whom both physician and patient assessments were available were evaluated. The percentages of patients assessing their global health worse than the physician rated disease activity were analysed for rheumatoid arthritis (RA, on average n≈6,554 each year), ankylosing spondylitis (AS, n≈1,079), psoriatic arthritis (PsA, n≈1,191), systemic lupus erythematodes (SLE, n≈800) and polymyalgia rheumatica (PMR, n≈489) with regard to sex, age, disease duration and education.
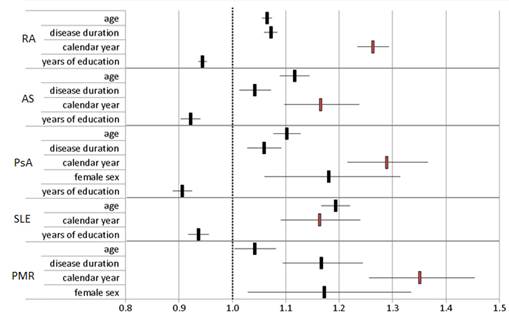
Results In 2000, patient ratings were on average 0.9-1.6 scores worse than physician ratings. These differences further increased by 0.4-1.2 score units until 2012. In 2000, patient ratings at least one score worse than physician ratings were found in 62-65% of patients with RA, AS, PsA and PMR, and in 53% of patients with SLE. We saw an increase in poorer patient ratings by 12-16% for all diagnoses but AS (+7%) between 2000 and 2012. Male patients showed a stronger increase in discrepant ratings over time. Patients aged up to 40 had a higher agreement between physicians and patients than older patients. Poorer patient ratings were more frequent in patients with longer disease duration and lower education. The higher rates with both increasing age and disease duration are probably also reflecting the burden of co-morbid conditions. When analysing by logistic regression which parameters predict a poorer patient than physician rating, calendar year played a significant role in all diagnosis groups after adjusting for sex, age, disease duration and education.
Conclusion The discrepancies between patient and physician ratings have increased over the past decade for various diagnoses. In addition to a rising importance of quality of life in public perception in recent years, in times of almost universal internet access this might also reflect the better informed patient with higher expectations. These changes should be taken into account when comparing patient reported outcomes over long periods. In general, our findings underline the need to consider carefully the patient view when assessing treatment outcomes.
Figure 1: Predictors of a poorer patient than physician rating (odds ratios with 95% confidence interval); age, disease duration and calendar year in 5-years steps
Disclosure:
D. Huscher,
None;
K. Albrecht,
None;
K. Thiele,
None;
S. Bischoff,
None;
A. Krause,
None;
S. Späthling-Mestekemper,
None;
S. Wassenberg,
None;
A. Zink,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increasing-discrepancies-between-physician-assessment-of-disease-activity-and-patient-global-health-in-germany-between-2000-and-2012/