Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: SLE disproportionately affects individuals of African (AA) compared to European ancestry (EA). In addition to a higher incidence, the disease is more severe in patients of AA; they have a higher burden of renal comorbidities such as end stage renal disease (ESRD) and others (1). A high risk (HR) genotype in apolipoprotein L1 (APOL1), present in 13% of AA and absent in EA individuals, is associated with increased risk of renal and hypertensive disorders in populations of AA. APOL1 expression is driven by interferon and the HR genotype is more common in patients with lupus nephritis (LN)-ESRD. We examined the hypothesis that the APOL1 HR genotype is responsible for the increased prevalence of renal comorbidities in SLE patients of AA compared to those of EA.
Methods: We performed a retrospective cohort study in patients with SLE of EA and AA at a tertiary hospital using de-identified genetic and electronic health record (EHR) data. Ancestry was defined by principal components (PCs) and HapMap references. We assessed the prevalence of clinical conditions in the EHR using ICD9 and ICD10 diagnosis codes. Highest serum creatinine was extracted as a measure of renal function. Genotyping was performed with the Illumina Infinium® Expanded Multi-Ethnic Genotyping Array to define APOL1 risk genotypes: HR genotypes were defined as G1/G1, G2/G2, or G1/G2 and low risk as carriers of 1 or 0 copies of the G1 or G2 alleles. The prevalence of clinical disorders was compared in patients with SLE: EA vs. all AA; EA vs. AA excluding those with the APOL1 HR genotype (with a PheWAS approach), and AA APOL1 HR vs low risk (LR) genotypes (with logistic regression for selected diagnoses). Covariates included sex, year of birth, age at SLE diagnosis, follow-up in the EHR, and 5 PCs.
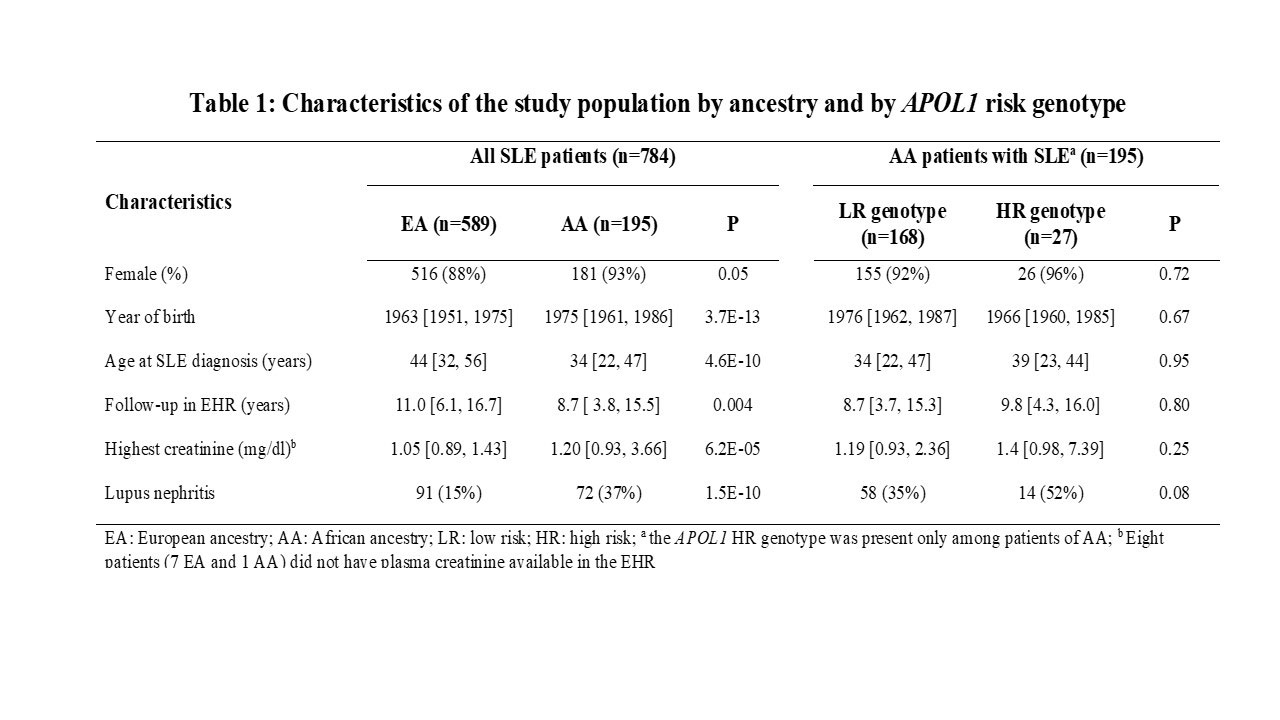
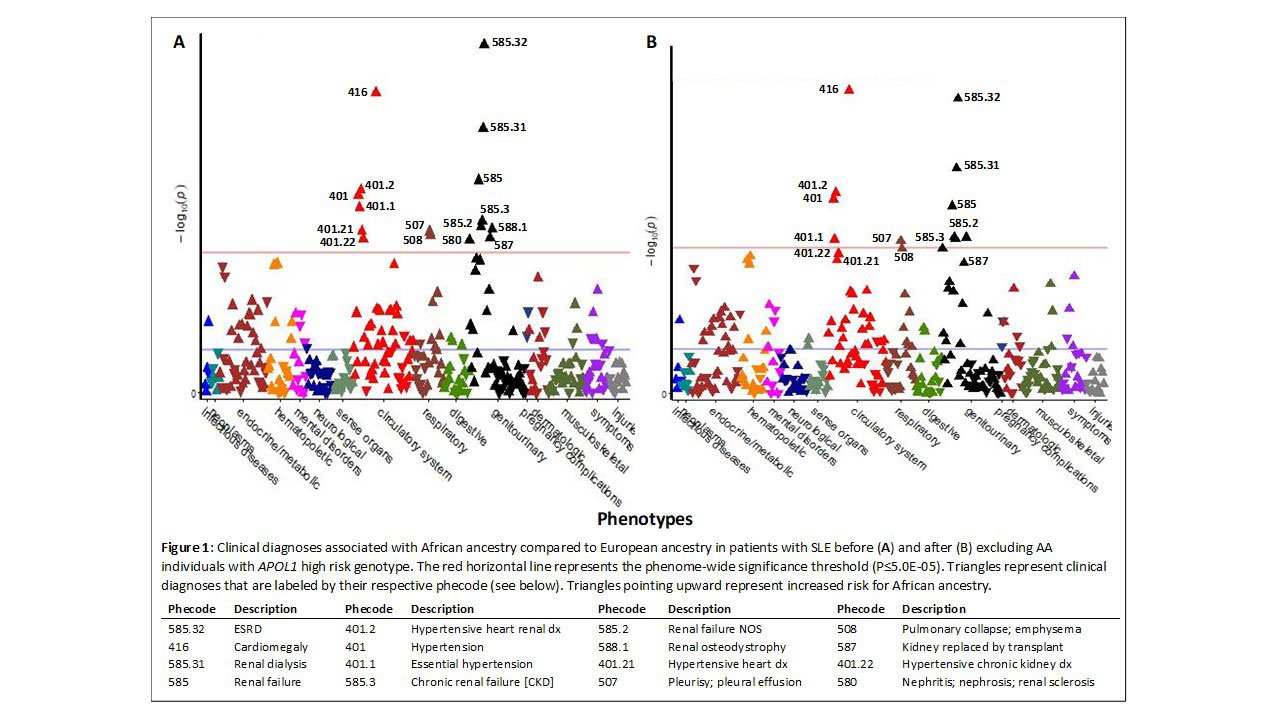
Results: We studied 784 patients with SLE; 25% were of AA. The APOL1 HR genotype was absent in patients of EA and present in 27 (13.8%) patients of AA. Patients of AA were younger, diagnosed at earlier age, had a higher prevalence of LN, and had higher peak creatinine levels compared to EA patients; however, in APOL1 HR and LR genotypes, only the difference in the prevalence of LN (52% vs. 35%, respectively) approached statistical significance (Table 1). In the PheWAS, 16 diagnoses were significantly more common in AA than EA patients (P≤ 5E-05, Fig 1A); all these diagnoses were renal or renal-related. Excluding individuals with the APOL1 HR genotype had minor effects on the comparison between EA and AA patients; 11 of the 16 diagnoses remained more common in AA than EA patients at phenome-wide significance (P≤5E-05, Fig. 1B), and the remaining 5 diagnoses had P< 0.0002. In patients of AA, none of the 16 renal-related diagnoses of interest were significantly higher in patients with the HR genotype (P >0.05).
Conclusion: In SLE, the higher prevalence of renal and hypertensive disorders in those of AA compared to EA was not explained by the presence of APOL1B high risk variants.
Reference
1. Barnado A, et al. Phenome-wide association study identifies marked increased in burden of comorbidities in African Americans with systemic lupus erythematosus. Arthritis Res Ther. 2018;20:69.
To cite this abstract in AMA style:
Karakoc G, Liu G, Gamboa J, Chung C, Mosley J, Stein M, Kawai V. Increased Risk of Adverse Renal Outcomes in Patients of African Ancestry with Systemic Lupus Erythematosus (SLE) – Role of APOL1 [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/increased-risk-of-adverse-renal-outcomes-in-patients-of-african-ancestry-with-systemic-lupus-erythematosus-sle-role-of-apol1/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-risk-of-adverse-renal-outcomes-in-patients-of-african-ancestry-with-systemic-lupus-erythematosus-sle-role-of-apol1/