Session Information
Date: Tuesday, October 23, 2018
Title: 5T111 ACR Abstract: SLE–Clinical IV: Clinical Outcomes (2892–2897)
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Methods: We conducted a population-based case-control study using an administrative health database including the entire population in the province of British Columbia, Canada (over 5 million individuals). We identified cases with SLE who died, and for each case we identified up to three living controls with SLE matched on age, sex, and SLE disease duration. We used conditional logistic regression to assess the association between current use of HCQ or recent discontinuation of HCQ and the risk of all-cause and cause-specific mortality relative to remote HCQ users. Remote users were defined by a duration greater than 365 days between the last HCQ prescription and the index date (i.e., death date). Recent users had a duration less than 365 days since the last HCQ prescription and index date. Current users had active HCQ prescriptions spanning the index date. Fully adjusted models included chronic kidney disease, Charlson comorbidity index, glucocorticoids, and cardiovascular medication use assessed at the time of SLE diagnosis.
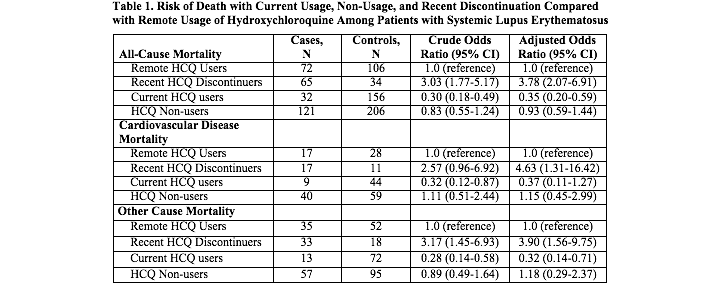
Results: We identified 290 SLE cases who died and 502 matched controls among 792 individuals with SLE. The mean age at index date was 65.6 years for cases and 64.7 years for controls. The majority were female (87.9% of cases and 91.4% of controls). The mean SLE disease duration was 5.3 years for both groups. Adjusted odd ratios (ORs) for all-cause mortality relative to the remote users were 0.35 (95% CI: 0.20, 0.59) for current users and 3.78 (95% CI: 2.07, 6.91) for subjects who recently discontinued HCQ (Table 1). HCQ non-users had the same risk of death as remote users (OR 0.93 [95% CI: 0.59, 1.44]). Similar trends were seen for the risk of mortality due to CVD.
Conclusion: In this general population-based case-control study of SLE mortality, we found a nearly four-fold increased risk of death associated with recent HCQ discontinuation and a substantially increased risk of CVD death. The cause of this association is unknown. This could be partially explained by a direct protective effect of HCQ that is rapidly lost following discontinuation. However, there may also be an indirect association due to selective provider discontinuation or patient non-adherence with HCQ when patients become acutely ill. We also demonstrated a 65% reduced risk of death among current HCQ users compared with remote users. By leveraging remote users as the comparison group, we reduced the potential for confounding by indication. Further studies are needed to explain the temporal relationship between HCQ discontinuation and SLE mortality.
To cite this abstract in AMA style:
Jorge A, Lu N, Sayre EC, Tavakoli H, McCormick N, Esdaile JM, DeVera M, Choi HK, Avina-Zubieta JA. Increased Mortality Among Patients with Systemic Lupus Erythematosus after Hydroxychloroquine Discontinuation [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/increased-mortality-among-patients-with-systemic-lupus-erythematosus-after-hydroxychloroquine-discontinuation/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-mortality-among-patients-with-systemic-lupus-erythematosus-after-hydroxychloroquine-discontinuation/