Session Information
Date: Monday, November 8, 2021
Title: Abstracts: Reproductive Issues in Rheumatic Disorders (1464–1467)
Session Type: Abstract Session
Session Time: 4:30PM-4:45PM
Background/Purpose: Studies show increased risks of adverse pregnancy outcomes in SLE patients. Few studies have investigated postpartum outcomes in these patients. Using a large, de-identified electronic health record (EHR), we estimated rates of postpartum infection, blood transfusion, and hospital length of stay and compared them to rates in controls without autoimmune disease. We also assessed for postpartum flares in SLE mothers.
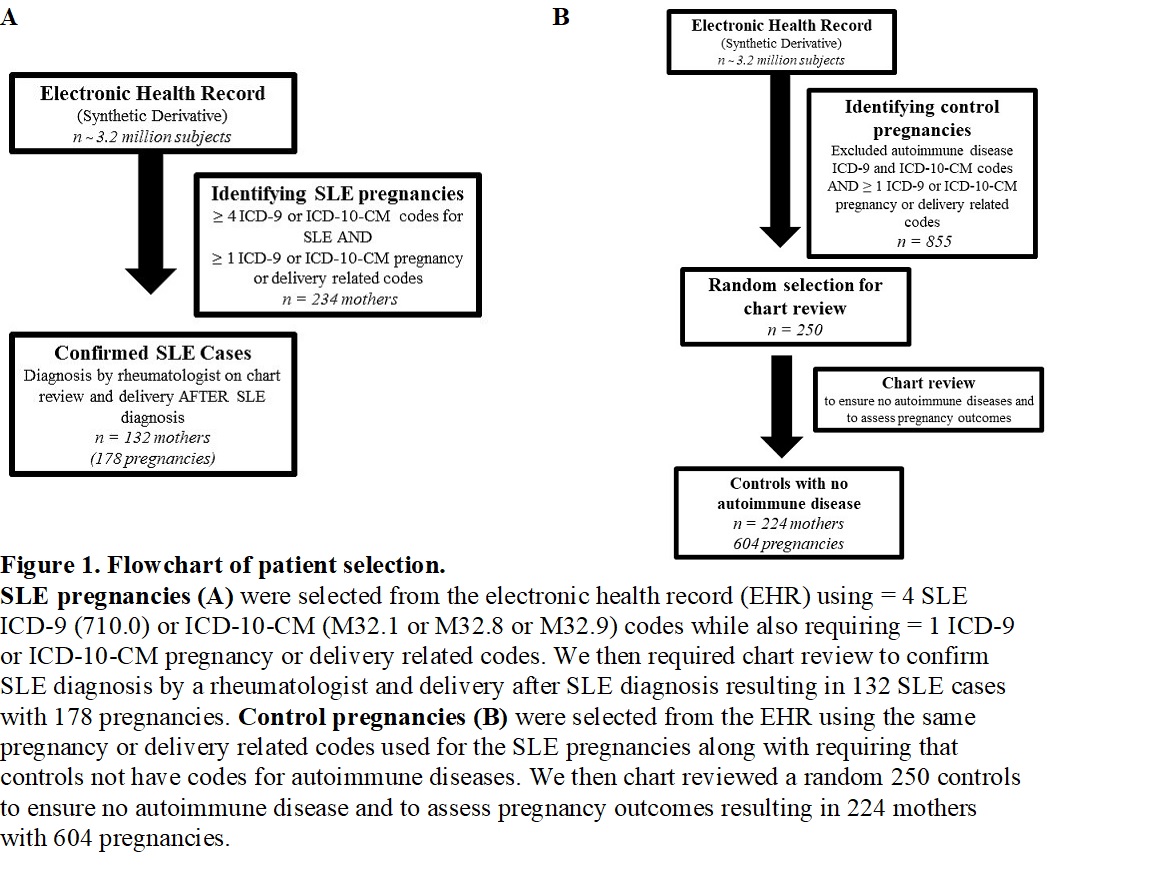
Methods: Using a large, de-identified EHR with over 3.2 million subjects, we identified deliveries to SLE mothers using a validated and published algorithm. This algorithm has a positive predictive value of 90% and uses ≥ 4 SLE ICD-9 or ICD-10-CM codes and ≥ 1 validated, delivery-related codes. We performed chart review to confirm SLE diagnosis by a rheumatologist and focused on SLE deliveries after SLE diagnosis. We assessed for SLE medication use at a postpartum visit between 6 weeks to 3 months after delivery. We identified control mothers without autoimmune disease ICD-9 or ICD-10-CM codes and the same delivery-related codes used to identify SLE deliveries. We then randomly selected 250 control mothers for chart review to ensure they did not have autoimmune disease. A flowchart is shown in Figure 1. Postpartum infection was defined as infection documented by a physician from delivery to 6 weeks postpartum. Blood transfusions were assessed during the admission for delivery. SLE flares were defined as the rheumatologist documenting a flare or increase in disease activity in notes from delivery to 6 months postpartum. Length of stay was days from admission to discharge.
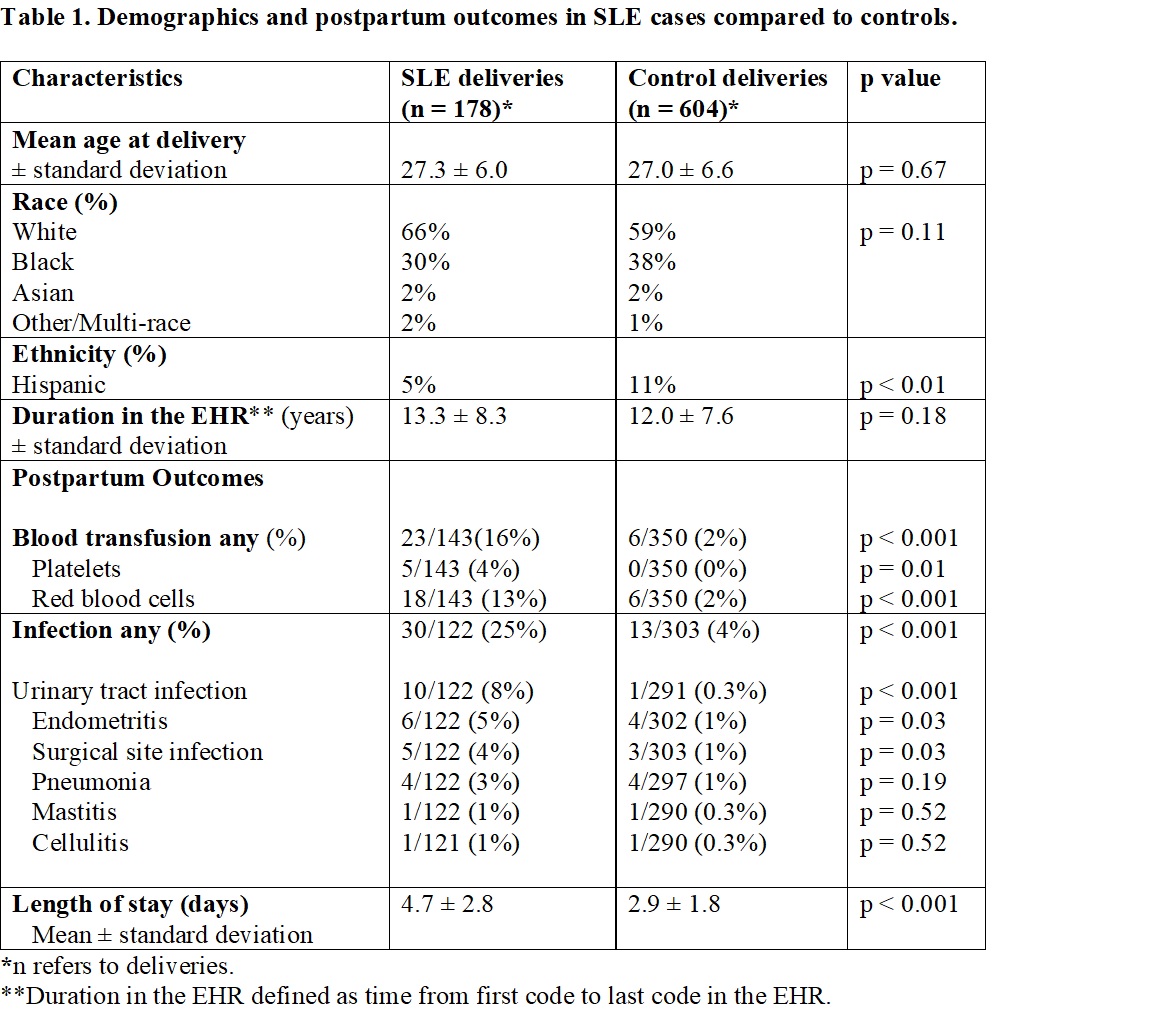
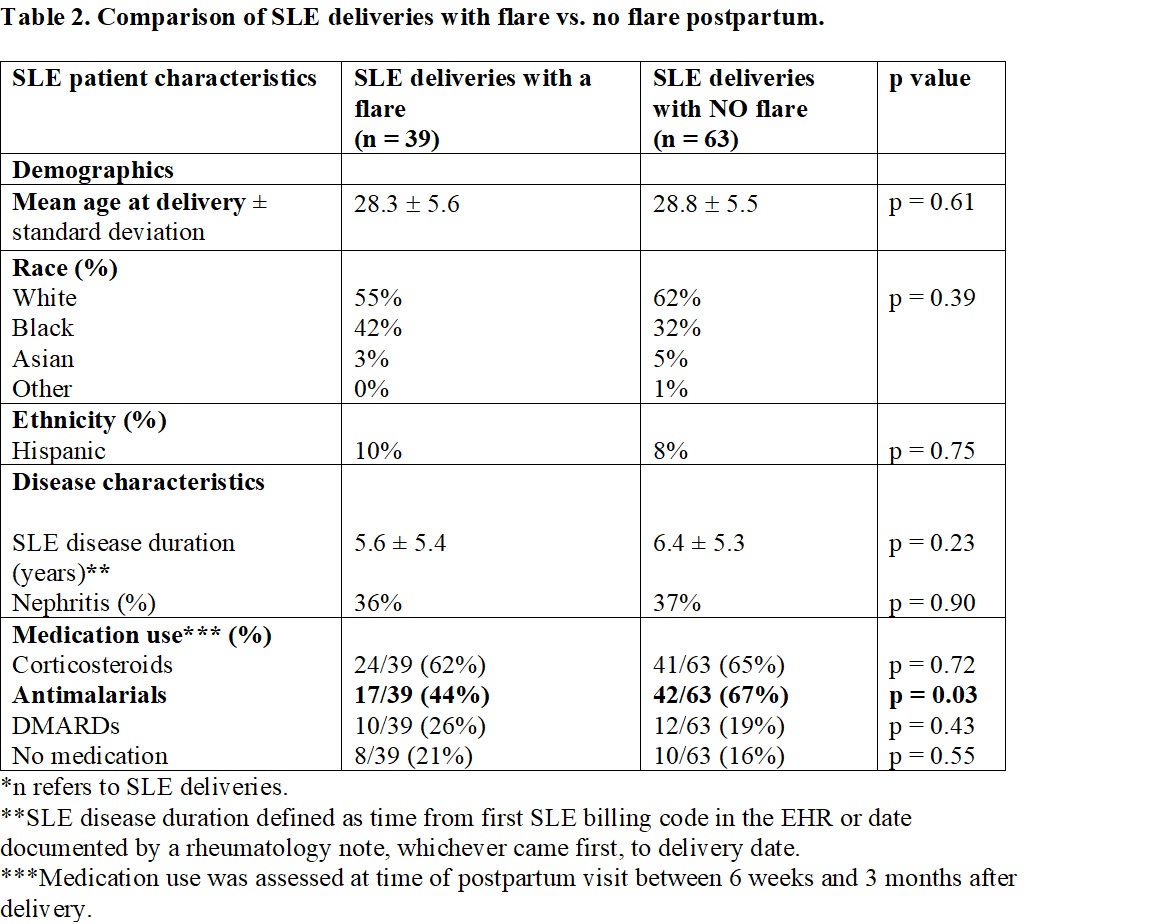
Results: We identified 178 pregnancies after SLE diagnosis to 132 SLE mothers and 604 pregnancies to 224 control mothers without autoimmune disease. Our SLE and control mothers had similar mean age at delivery (27.0 ± 6.6 vs. 27.3 ± 6.0, p = 0.67) and a similar racial/ethnic makeup that was predominantly White (66% vs. 59%, p = 0.11) (Table 1). Blood transfusion rates were significantly higher in SLE cases vs. controls (16% vs. 2%, p < 0.001) (Table 1). Postpartum infection rates for any infection were significantly higher in SLE cases vs. controls (25% vs. 4%, p < 0.001). Hospital length of stay was significantly longer in SLE cases vs. controls (4.7 ± 2.8 vs. 2.9 ±1.8, p < 0.001). For SLE cases, postpartum flare rate was 38%. We compared SLE deliveries with a disease flare vs. deliveries without a flare (Table 2). There were no significant differences in age, race, ethnicity, SLE nephritis, or SLE disease duration. For deliveries without a flare, mothers were more likely to be on antimalarials compared to deliveries with a flare (67% vs. 44%, p = 0.03). Flares were managed by adding or increasing corticosteroids (79%), adding an antimalarial (16%), adding or titrating a DMARD (11%), although 11% had no change to medications.
Conclusion: Our study demonstrates that SLE patients are at an increased risk for adverse postpartum outcomes compared to controls including infections, blood transfusions, and longer lengths of stay. We observed frequent flares postpartum with patients being more likely to flare if not prescribed antimalarials postpartum. This finding emphasizes the importance of antimalarials in the postpartum period to reduce flares.
To cite this abstract in AMA style:
Barnado A, Hubbard J, Green S, Osmundson S. Increased Adverse Maternal Postpartum Outcomes in Systemic Lupus Erythematosus Pregnancies Compared to Controls [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/increased-adverse-maternal-postpartum-outcomes-in-systemic-lupus-erythematosus-pregnancies-compared-to-controls/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-adverse-maternal-postpartum-outcomes-in-systemic-lupus-erythematosus-pregnancies-compared-to-controls/