Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Lymphopenia is common in patients with systemic lupus erythematosus (SLE), occurring in 75-90% of cases over the disease course. It can result from SLE activity, infections, or medications (glucocorticoids and immunosuppressants). There are no specific guidelines for managing SLE with lymphopenia. The objective of this retrospective study is to assess the incidence, risk factors and outcomes of severe lymphopenia (SL) in SLE.
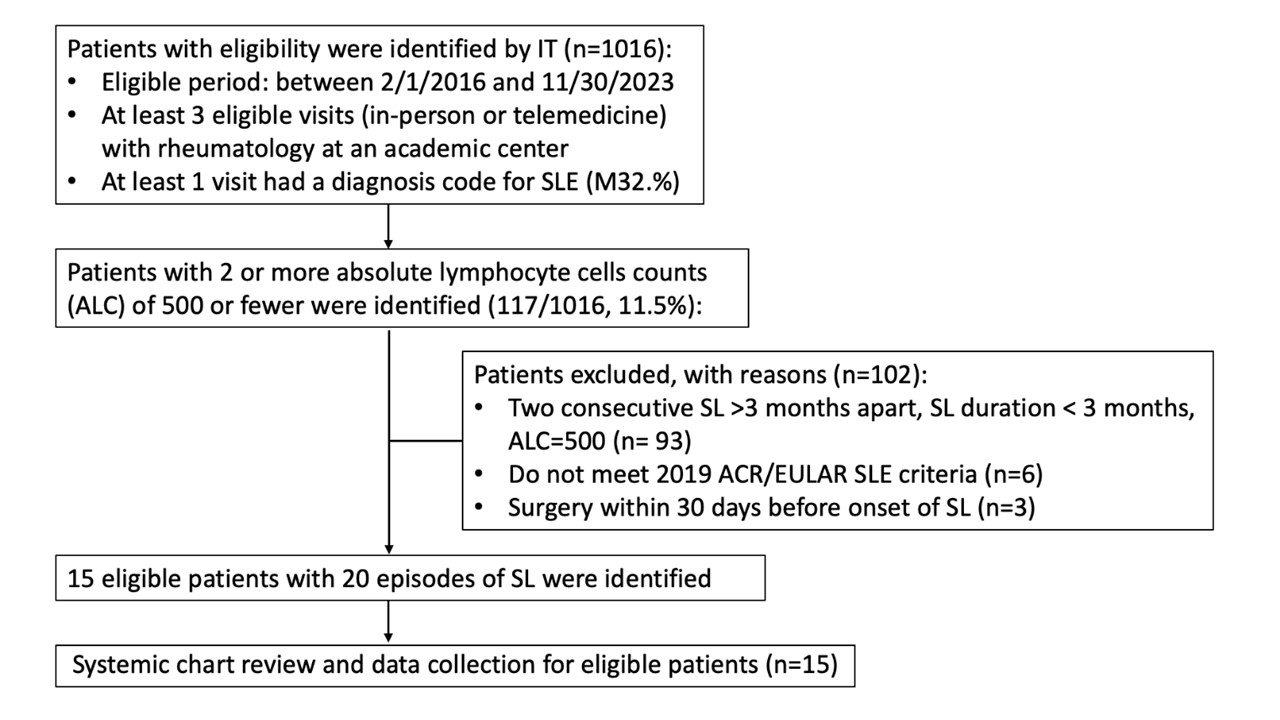
Methods: The records of SLE patients with SL seen at an academic medical center between 2/1 2016 and 11/30/2023, were retrospectively reviewed (Figure 1). Various disease parameters were compared six months before the onset of SL and during SL period in the eligible patients. Severe lymphopenia (SL) was defined as absolute lymphocyte counts (ALC) < 500/µL in at least two consecutive tests within a three-month period, with a duration of at least three months. The 2019 ACR/EULAR criteria were used to confirm the diagnosis of SLE.
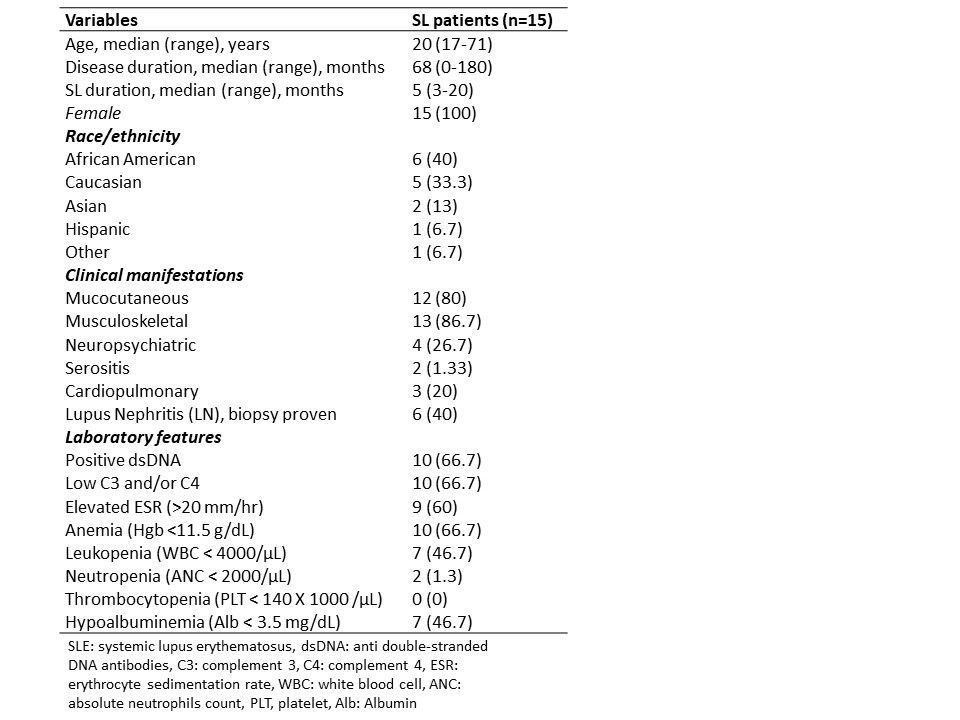
Results: Among 1,016 SLE patients, 117 (11.52%) experienced marked lymphopenia (ALC ≤ 500). There were 15 patients with 20 episodes of SL. All 15 patients were female, with a median age of 20 years (range: 17-71 years), a median disease duration of 68 months (range: 0-180 months), and a median SL duration of 5 months (range: 3-20 months). The majority were non-Caucasian (10/15, 66.7%). These patients had active SLE, as indicated by their serology and inflammatory markers (Table 1). Lupus nephritis was observed in 40% of patients.
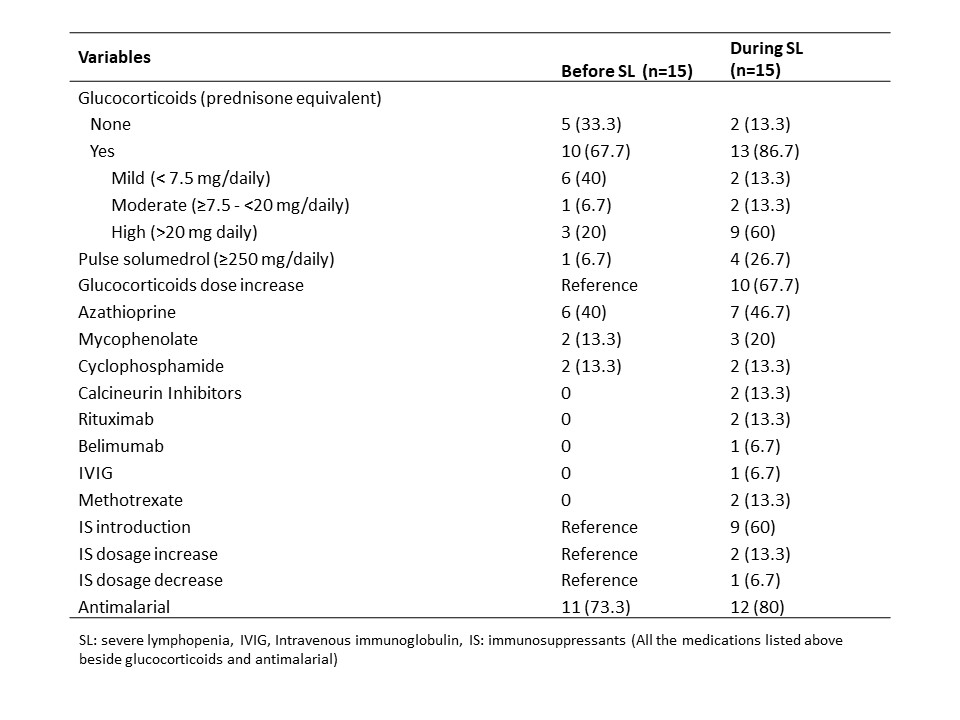
All patients had lymphopenia before progressing to SL, with ALC (mean± SD) decreasing from 605.2 ± 84.4 to 326.3 ± 70.63. Notably, there were no significant differences in laboratory values (C3, C4, ESR, Hgb, WBC, ANC, platelet count, ALT, AST, albumin, creatinine) before and during SL. Glucocorticoid use increased during SL compared to before (Table 2), with 10 patients (66.7%) requiring an escalation of glucocorticoid doses. Additionally, nine patients (60%) had new introductions of immunosuppressants (IS), and 2 patients (13.3%) had increased doses of IS during SL. One patient (6.7%) had a reduced azathioprine dose due to leukopenia during SL.
Prophylaxis for Pneumocystis jirovecii pneumonia (PJP) was administered to 20% of patients both before and during SL. During severe lymphopenia, four patients (26.7%) experienced 12 episodes of infection, primarily genitourinary tract infections, followed by cellulitis and lymphadenitis. No infections were reported before severe lymphopenia, and no opportunistic infections were observed before or during the period of SL.
Conclusion: In this cohort study, the majority of patients had active SLE and mild lymphopenia before the onset of SL, and they were predominantly non-Caucasian. SL was likely associated with the escalation of glucocorticoid and immunosuppressant use. More infections were observed during SL period; however, it is unclear whether these infections were due to the SL itself or the increased immunosuppression. No opportunistic infections were observed.
SLE: systemic lupus erythematosus, SL: severe lymphopenia,
ACR: American college of rheumatology,
EULAR: European league against rheumatism
To cite this abstract in AMA style:
Chen C, Wu E, Do H, Kirou K. Incidence, Risk Factors, and Outcomes of Severe Lymphopenia in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/incidence-risk-factors-and-outcomes-of-severe-lymphopenia-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-risk-factors-and-outcomes-of-severe-lymphopenia-in-systemic-lupus-erythematosus/