Session Information
Date: Sunday, October 26, 2025
Title: (0731–0764) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Ischemic vision loss affects up to one quarter of patients with giant cell arteritis (GCA). The incidence of ischemic vision loss among patients with isolated polymyalgia rheumatica (PMR) is poorly defined. This study aimed to quantify the risk of ischemic vision loss among patients with PMR, GCA, and matched population controls.
Methods: We conducted a retrospective cohort study using the US-based TriNetX electronic health records network. Adults ≥50 years were included if they had ≥2 ICD-9/10-CM codes for GCA or PMR, ≥1 year of prior follow-up, and a prednisone prescription within 30 days of their first diagnostic code. Matched general population control cohorts for PMR and GCA were constructed using 1:3 nearest-neighbor matching on the following variables: sex, race/ethnicity, regional location, birth year, year of cohort entry, and year of cohort exit. The primary outcome was ischemic vision loss, which was defined by ICD-9/10 codes for ischemic optic neuropathy and retinal artery occlusion. Multivariable Cox proportional cause-specific adjusted hazard ratios (aHR) and 95% confidence intervals (CI) were calculated to define the risk of ischemic vision loss.
Results: Of 56,899 patients, 16,001 had PMR, 3,054 had GCA, and 37,844 were matched controls. Median follow-up time was 3.4 years (interquartile range, 1.4-6.2). The incidence of ischemic vision loss over the entire follow-up period (10 years) was highest for GCA (9.2 per 1,000 person-years) followed by PMR (1.7 per 1,000 person-years), GCA controls (1.5 per 1,000 person-years), and PMR controls (1.4 per 1,000 person-years). Ischemic vision loss was increased in GCA as compared to PMR (aHR 5.36, 95% CI 4.09–7.02) and GCA as compared to matched-controls (aHR 5.69, 95% CI 3.95–8.18). No significant differences were observed for PMR as compared to matched controls (aHR 1.10, 95% CI 0.86–1.41). Sensitivity analyses over the first one year and the first 5 years of therapy supported the primary analyses.
Conclusion: In this large retrospective cohort study, patients with PMR had no increased risk of ischemic vision loss as compared to the general population or to patients with GCA. In contrast, patients with GCA were significantly more likely to suffer ischemic vision loss. These findings support the current approach of ophthalmology referral for patients with GCA and screening by symptoms alone for PMR.
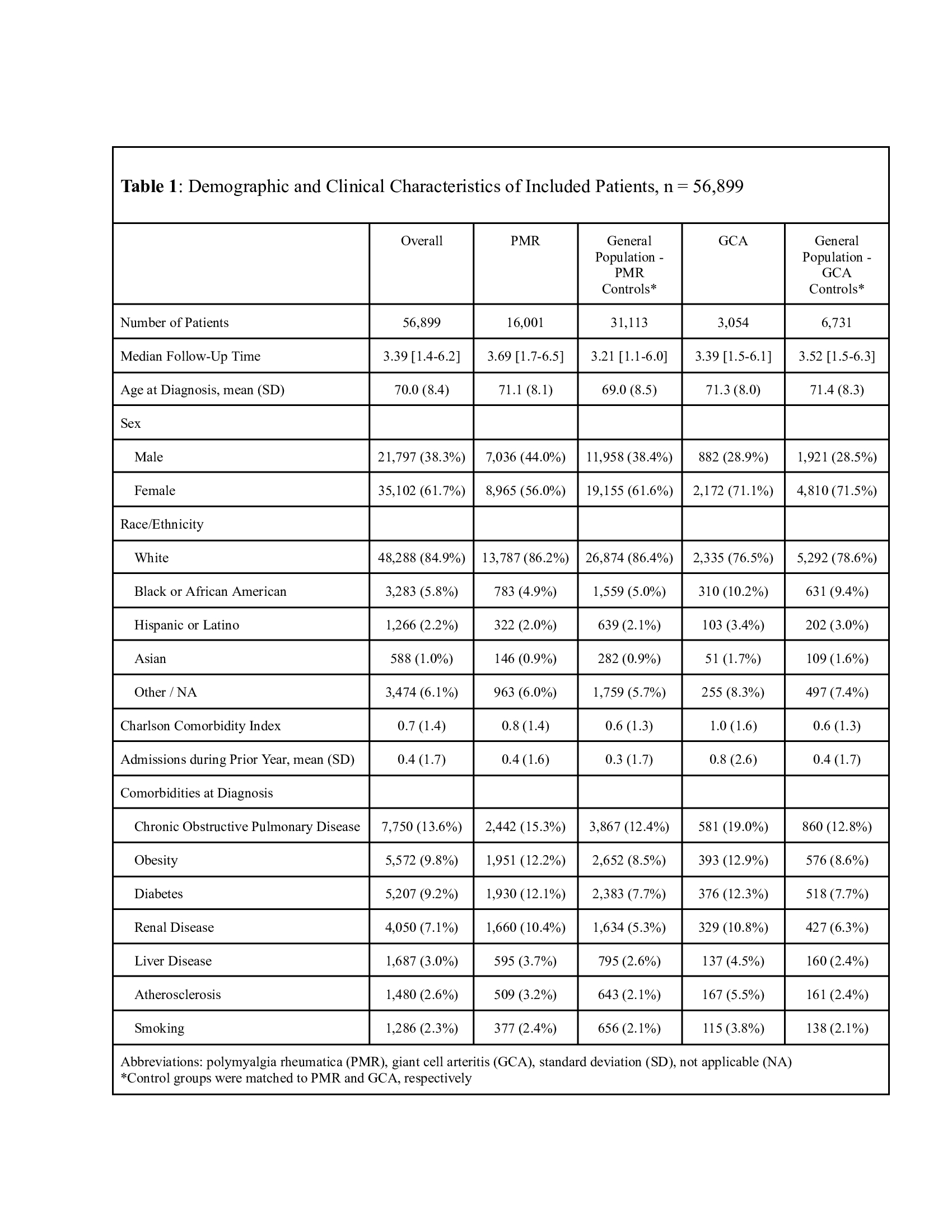 Demographics and Clinical Characteristics of Included Patients
Demographics and Clinical Characteristics of Included Patients
.jpg) Unadjusted Incidence of Ischemic Vision Loss Among Included Patients
Unadjusted Incidence of Ischemic Vision Loss Among Included Patients
.jpg) Cumulative Incidence of Ischemic Vision Loss Among Patients with GCA, PMR, and Matched Controls
Cumulative Incidence of Ischemic Vision Loss Among Patients with GCA, PMR, and Matched Controls
To cite this abstract in AMA style:
Peng M, Carlson K, Sattui S, Putman M. Incidence of Ischemic Vision Loss Among Patients with Polymyalgia Rheumatica and Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/incidence-of-ischemic-vision-loss-among-patients-with-polymyalgia-rheumatica-and-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-of-ischemic-vision-loss-among-patients-with-polymyalgia-rheumatica-and-giant-cell-arteritis/
