Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid Syndrome (APS) is classified into primary and secondary; the latter being associated with connective tissue disease. Systemic lupus erythematosus (SLE) is the most common cause of secondary APS, and the prevalence of antiphospholipid antibodies (APLAs), in patients with SLE is reported to be as high as 30% to 50% (1). The aim of our study was to determine what percentage of our SLE patients have had a complete APLA profile with or without thrombosis. We also looked at the timing these antibodies were obtained in regard to thrombotic events.
Methods: We reviewed EMR of patients with a diagnosis of SLE from 2012-2022. Data was obtained on presence or absence of antiphospholipid antibodies testing in these patients along with the timing of these tests in relation to thrombotic events. Deep vein thrombosis, Cardiovascular accidents, Pulmonary Embolism and History of Miscarriages were few of the thrombotic events included for review.
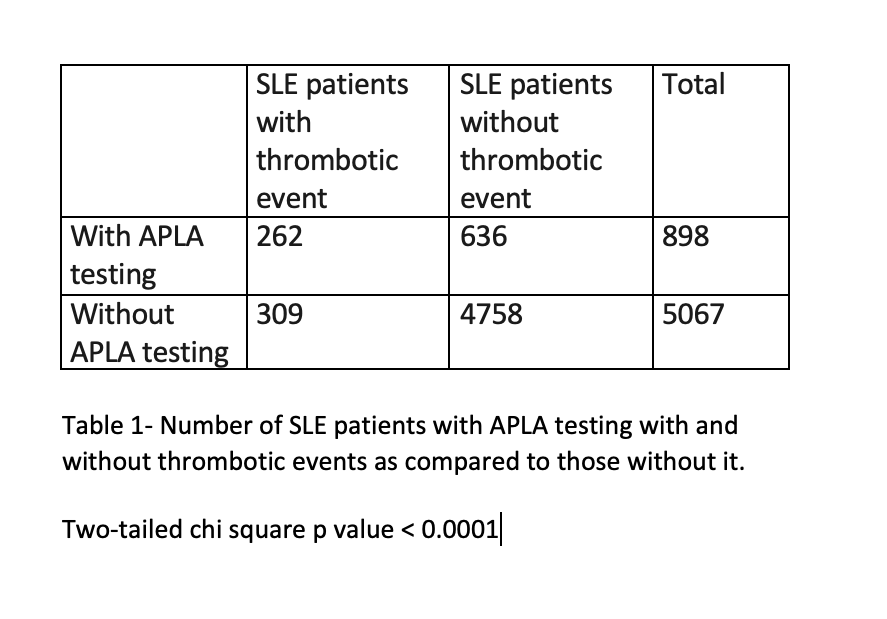
Results: A total of 5965 patient’s charts were used for analysis. 5207 of these were females. Only 898 (15%) patients were found to have an entire antiphospholipid antibodies panel tested in them. 571 of SLE patients had a thrombotic event and 309 of these were without an APLA panel prior to the event. When number of SLE patients who had APLA testing done with and without thrombotic events were compared to those without APLA testing, the results were found to be statistically significant. (p value < 0.0001 ; Table 1).
Conclusion: Despite the increased risk of APS and thrombosis in patients with SLE, there is inadequate screening with antiphospholipid antibodies in these patients. Most of the times antibody testing in these patients is driven by a thrombotic event. We purpose an EMR alert to obtain antiphospholipid antibodies testing in all SLE patients who are without one to better categorize their risk of APS and thrombosis.
To cite this abstract in AMA style:
Munawar t, Sherazi M, Perl A. Inadequate Screening for Antiphospholipid Syndrome with Antiphospholipid Antibodies in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/inadequate-screening-for-antiphospholipid-syndrome-with-antiphospholipid-antibodies-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inadequate-screening-for-antiphospholipid-syndrome-with-antiphospholipid-antibodies-in-patients-with-systemic-lupus-erythematosus/