Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) is a heterogeneous disease and its assessment is sometimes difficult. Perception of disease activity by patient and physician is frequently discordant in patients in clinical remission (1). Ultrasound (US) is an imaging technique, which can detect inflammation in PsA. The aim of our study was to assess whether persistence of disease activity evaluated by the patient, considered in remission by his rheumatologist, was associated with inflammation measured by US.
Methods: We performed a transversal monocentric study. PsA patients were included if they met the CASPAR criteria and were considered in remission by their rheumatologist. Demographic data, characteristics of the disease and treatments were collected. Discordance was defined by a difference between patient’s and rheumatologist’s global assessment ≥30/100 on a Visual Analogic Scale. An US examination was performed on 50 joints, 28 tendons and 14 entheses by an independent investigator. Synovial or tendon sheath hypertrophy and PD signal were evaluated on a semi-quantitative scale, B Mode and PD signal abnormalities on entheses were searched, according to the EULAR-OMERACT scoring system. US remission was defined by no power Doppler (PD) signal on joints, tendons and entheses and minimal US activity by maximum one PD signal on the same sites. Univariate and multivariate analyses were performed to evaluate factors associated with US abnormalities
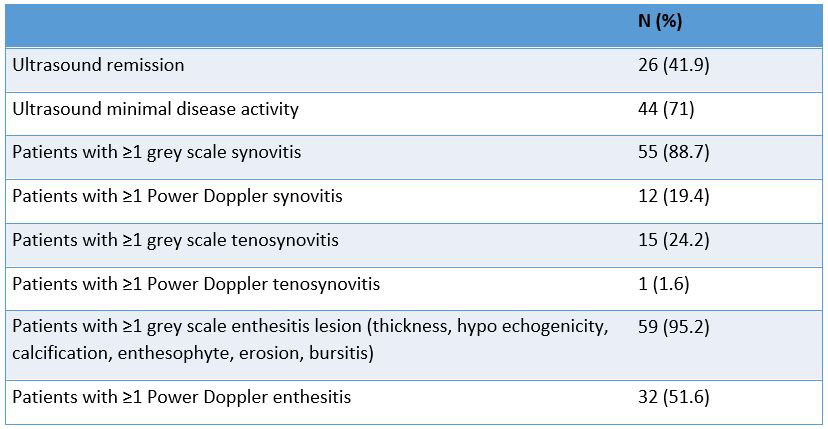
Results: Sixty-two PsA patients were included. 40.3% were women, the mean (SD) age was 55 (14) years, 42% were in US remission and 71% in minimal US activity (Table 1), 19.4% had ≥1 PD synovitis and 88.7% had a B mode synovitis, 95.2% had a B mode abnormality on entheses and 51.6% had ≥1 PD signal on entheses. Thirty nine percent had a discordant disease activity assessment with their rheumatologist. In univariate analysis, discordance was not associated with US remission (OR=1.71 (95%CI 0.61-4.83), p=0.224) or US minimal disease activity (OR=0.99 (95%CI 0.32-3.05), p=0.602). In multivariate analysis, US remission was independently associated with female gender (OR=3.94 (95%CI 1.20-12.9), p=0.024) and younger age (OR=0.95 (95%CI 0.91-0.99), p=0.027). Minimal US activity was associated with history of enthesis lesion (OR=11.26 (95%CI 1.34-94.93), p=0.026) and age (OR=0.95 (95%CI 0.90-1), p=0.044).
Conclusion: Our study showed persistent inflammation evaluated by US in PsA patients considered in remission by their rheumatologist. However, prevalence of residual inflammation evaluated by US was not higher in patients with self-assessment of their disease discordant from their rheumatologist.
To cite this abstract in AMA style:
Moly M, Lukas C, Morel J, Combe B, Mouterde G. In Psoriatic Arthritis Patients Considered in Remission by Their Rheumatologist, Can Discordance in Disease Activity Assessment Between Patient and Rheumatologist Be Explained by Residual Inflammation as Measured by Ultrasonographic Examination? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/in-psoriatic-arthritis-patients-considered-in-remission-by-their-rheumatologist-can-discordance-in-disease-activity-assessment-between-patient-and-rheumatologist-be-explained-by-residual-inflammation/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-psoriatic-arthritis-patients-considered-in-remission-by-their-rheumatologist-can-discordance-in-disease-activity-assessment-between-patient-and-rheumatologist-be-explained-by-residual-inflammation/