Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Registry data have shown that treatment with bDMARDs induces remission or LDA (RLDA) in up-to 50% of RA patients. Approximately 30-50% of patients have moderate disease activity (MDA) after treatment with bDMARDs, nevertheless data for this group are limited. We sought to assess long term outcome and characterize RA patients with persistent MDA (pMDA) on bDMARDs in clinical practice.
Methods:
We analyzed data from the University of Crete Rheumatology Clinic. Disease activity, function, treatments of all patients starting a bDMARD are recorded prospectively every 3-6 months. Herein, we included patients with at least 3 years of follow-up, irrespective of switches. If DAS28-ESR was at the same disease activity range for at least 50% of the follow-up time, patients were assigned to one of 3 groups: persistent RLDA (pRLDA), pMDA and persistent high disease activity (pHDA). HAQ at 3 years was the primary outcome, while baseline characteristics and predictors of pMDA were assessed.
Results:
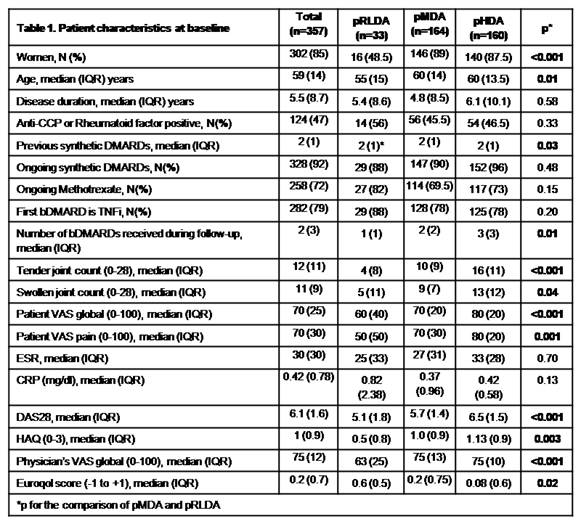
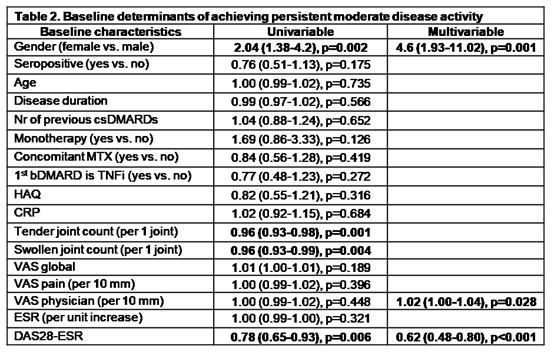
Out of 479 patients with complete data, 357 could be assigned to one of the aforementioned groups; 33,164 and 160 patients in pRLDA, pMDA and pHDA respectively. At baseline, pMDA patients were older, more often women, have received more csDMARDs and had higher DAS28, HAQ and EuroQol status compared to pRLDA group (Table 1). During follow-up, pMDA had more bDMARDs switches as compared to pRLDA [median (IQR) 1(2) vs 0(1), p=0.01]. Notably, although patients in pMDA had significant improvement in HAQ [baseline vs 36 months, median (IQR) HAQ: 1(0.9) and 0.5(0.8) respectively, p<0.001], HAQ at 3 years was significantly higher for pMDA compared to pRLDA group [0 (0.25) vs 0.50 (0.83), p<0.001] (Figure 1A). Of note, HAQ trajectories according to DAS28 grouping were clearly defined early at treatment course (6 months) and did not intersect throughout follow-up (Figure 1B). Multivariate analysis indicated that female sex, physician’s evaluation and DAS28 were independent predictors for clustering patients in the pMDA group (Table 2).
Conclusion:
In clinical practice 34% and 33% of RA patients on bDMARDs have persistent MDA or HDA in spite of bDMARDs switches. Although patients on pMDA present early significant improvement in HAQ, they still have worse functional status, compared to patients in pRLDA, after 3 years of follow up.
To cite this abstract in AMA style:
Genitsaridi I, Flouri I, Repa A, Avgoustidis N, Kougkas N, Papalopoulos I, Polia S, Marias K, Plexousakis D, Bertsias G, Sidiropoulos P. In Clinical Practice a Substantial Group of Rheumatoid Arthritis (RA) Patients on Biologic Therapy (bDMARDs) Has Persistent Moderate Disease Activity Despite Treatment Switches That Correlates with Unfavourable Long-Term Outcome [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/in-clinical-practice-a-substantial-group-of-rheumatoid-arthritis-ra-patients-on-biologic-therapy-bdmards-has-persistent-moderate-disease-activity-despite-treatment-switches-that-correlates-with-un/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-clinical-practice-a-substantial-group-of-rheumatoid-arthritis-ra-patients-on-biologic-therapy-bdmards-has-persistent-moderate-disease-activity-despite-treatment-switches-that-correlates-with-un/