Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: The risk of developing invasive pneumococcal pneumonia is 13 times higher in Lupus patients in comparison with general population. CDC anticipates 7.6 Million-Dollar medical cost reduction by providing pneumococcal vaccination per guidelines. Improving overall pneumococcal vaccination rate in lupus patients at our clinic through a multifaceted quality improvement initiative.
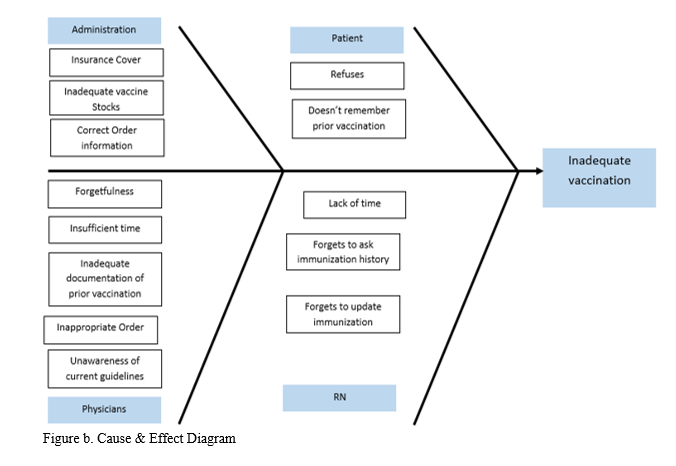
Methods: Eligibility: All lupus patients should receive pneumococcal vaccination. With help of quality improvement tools (interview with stakeholders {fig a}, process mapping) we analyzed the underlying barriers in providing vaccination and prepared a cause & effect diagram {fig b}. Following interventions were implemented, based on above analysis: Staff was responsible to confirm previous Pneumococcal vaccination, administer vaccines and update immunization history. Physicians were responsible to review daily reminders and place correct vaccination orders. Patients were given information handouts and education regarding Pneumococcal vaccines. After implementation of project, we calculated following rates (per week): Pneumococcal Vaccination (PCV 13, PCV 23 & vaccination complete) rates (percentage of pneumococcal vaccination given), documentation error rate (percentage of charts with immunization schedule not updated), historical error rate (percentage of patients not given pneumococcal vaccination due to unknown previous vaccination history) and vaccination refusal rate (percentage of patients refusing pneumococcal vaccination). Weekly progress was plotted on graph and discussed with the team members which helped us in modifying the interventions iteratively for achieving better rates.
Results: In 2 months {fig c}, overall vaccination improved from 8% to 28.2%, PCV 13 vaccination rate improved from 5% to 27.8%, PCV 23 vaccination rate improved from 8% to 50% and pneumococcal vaccination complete rate increased from 2% to 50%. Patient refusal rate decreased from 25% to 14%. 40% of patients are still not receiving immunization because of other reasons (forgetfulness, insufficient time).
Conclusion: Integrated workflow and performance data sharing helped in improving vaccination rates. Ongoing efforts are focused to overcome remaining barriers and achieve better rates.
To cite this abstract in AMA style:
Garg S, Lipson A, Tsagaris K. Improving the Overall Pneumococcal Vaccination Rate in Lupus Patients at the Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/improving-the-overall-pneumococcal-vaccination-rate-in-lupus-patients-at-the-rheumatology-clinic/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-the-overall-pneumococcal-vaccination-rate-in-lupus-patients-at-the-rheumatology-clinic/