Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Patients with rheumatologic diseases are frequently placed on immunosuppressant medications which increase their risk of developing Streptococcus pneumoniae infections. The Advisory Committee on Immunization Practices recommends that all immunosuppressed adults receive the 13-valent pneumococcal conjugate vaccine (PCV-13) followed by the 23-valent pneumococcal polysaccharide vaccine (PPSV-23) but many specialty clinics lack processes of care that facilitate immunization. The objective of this study was to improve pneumococcal immunization rates for patients on immunosuppressant medications in the adult rheumatology clinic.
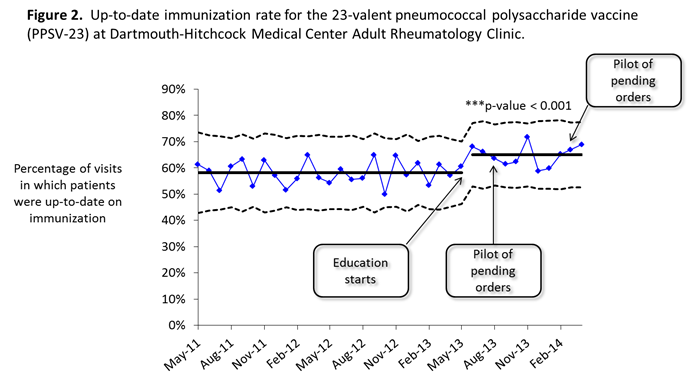
Methods: Immunization rates for PCV-13 and PPSV-23 were defined as the proportion of visits in which patients were up to date on their immunization. Data obtained from the electronic health record from May 2011 to April 2014 was analyzed using statistical process control methods. Rates over time were tracked using p-charts. Semi-structured interviews were performed with clinic staff to map the processes for immunization and create cause-and-effect diagrams. Interventions consisted of staff and provider education, a standardized process for obtaining immunization histories and a standing order permitting clinical support staff to order and administer immunizations via a protocol.
Results: At baseline, there was no standardized process for assessing immunization histories or providing immunizations in the clinic. Barriers included provider knowledge gaps, uncertainty regarding whether specialists or primary care providers should immunize, missing immunization records, lack of reminders and lack of time. The interventions resulted in statistically significant increases in the PCV-13 immunization rate from 3.0% to 33.3% (p-value < 0.001) and the PPSV-23 immunization rate from 58.1% to 64.9% (p-value < 0.001).
Conclusion: Rheumatologists place many patients on immunosuppressant medications rendering them high risk for infection yet many clinics have not incorporated immunizations into their standard processes. Standing orders combined with education should be considered as a potential intervention.
Disclosure:
L. Dudley,
None;
S. Liu,
None;
K. Merrihew,
None;
J. Verrill,
None;
L. Brown,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-pneumococcal-immunization-rates-for-patients-on-immunosuppressant-medications-at-an-academic-rheumatology-clinic/