Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Systemic lupus erythematosus (SLE) affects both adults and children with an estimated prevalence in children of 8/100,000. More than 1000 deaths related to SLE occur in a 5-year period, with most common causes attributed to active disease and organ failure. Adequate control of the disease reduces risk of organ damage, which is more common in children. Reliable measurement and documentation of disease activity is a key initial step for disease control. To achieve proper documentation of disease activity, our team developed a disease activity assessment tool called the Lupus Care Index (LCI). This index utilizes three existing metrics: SLE disease activity index (SLEDAI), Physician global assessment (PGA), and patient pain score. At our institution, we found that only one third of children diagnosed with SLE (cSLE) had proper documentation of all three components of LCI. We implemented a quality improvement (QI) project with aim to increase Lupus Care Index documentation, in children with SLE, from 38 % to 80%, by June 30, 2018.
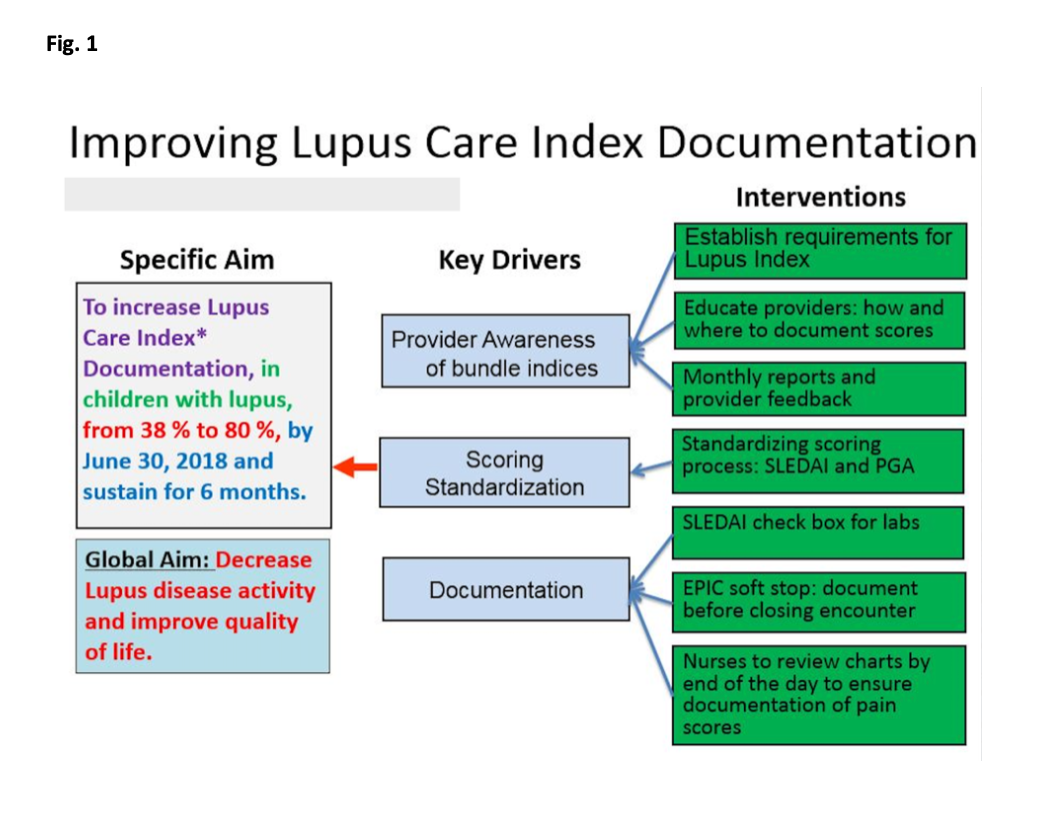
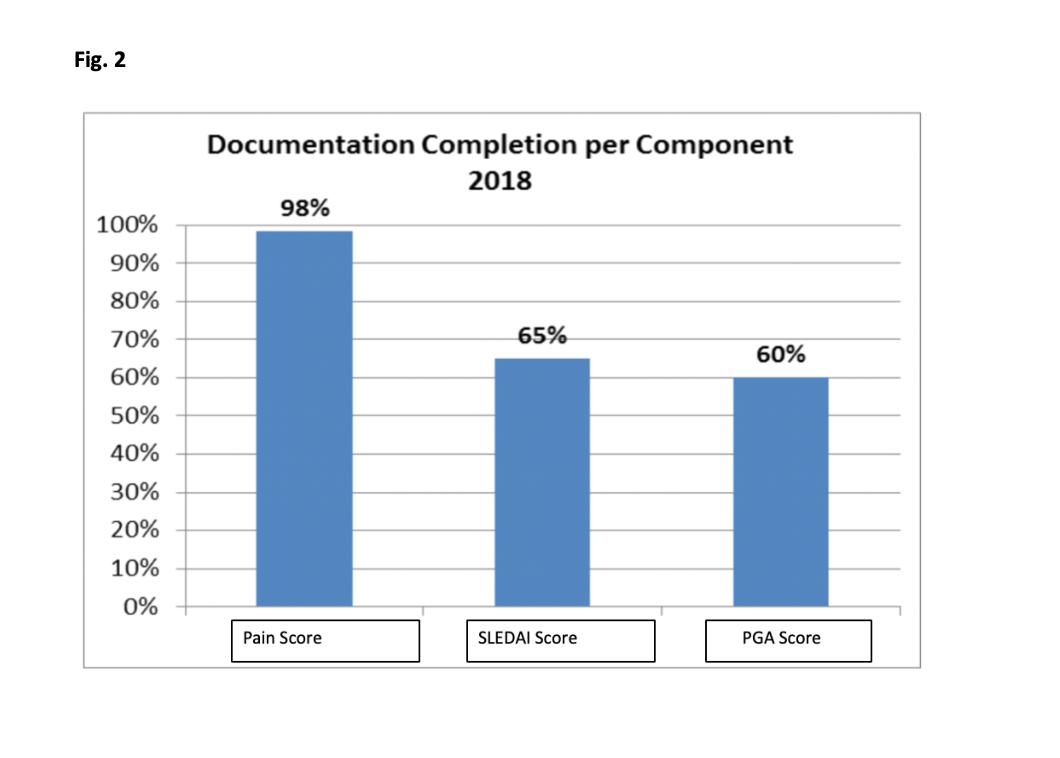
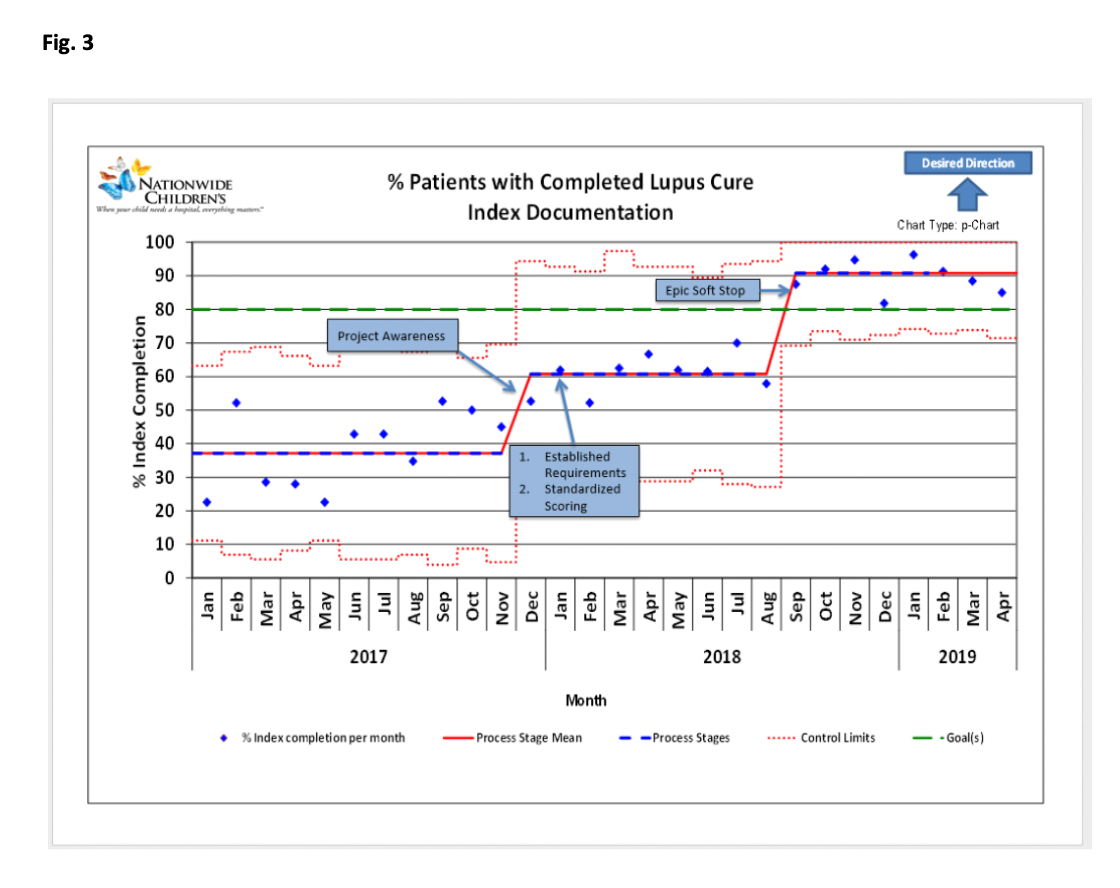
Methods: We established a QI team including physicians, nurses, QI support staff. Patients with cSLE who received medical care in the pediatric rheumatology clinic from January 1, 2016 to November 31, 2016 were included in the baseline analysis. We excluded clinic visits scheduled for teaching purposes. Our process included a brainstorming session followed by development of a key driver diagram (Fig. 1). Our first PDSA cycle focused on establishing requirements for LCI and a team consensus for proper documentation. Next, we created a Pareto chart to assist with a targeted intervention approach focusing on least documented indices (Fig. 2). We ran monthly reports and provided timely feedback to providers, and developed EHR (electronic health medical record; EPIC) “soft stop” reminders for physicians to document disease activity prior to closing clinic encounters. We utilized control charts to show the monthly percentage of c-SLE patients who had complete documentation of all three components of LCI (Fig. 3).
Results: We noted initial improvement trend in documentation with project awareness, score standardization, and provider level monthly feedback. However, we were able to achieve and surpass our goal of 80% in Aug 2018 after establishing the EHR soft stop reminder. We have sustained the desired improvement for 8 months.
Conclusion: The results of this quality improvement initiative highlight the role of EHR reminders along with provider feedback and transparency in promoting quality of health care delivery. Future directions of this project aim at utilizing the documented disease activity indices to reduce disease activity and improve patient disease outcomes.
To cite this abstract in AMA style:
Barbar-Smiley F, Lemle S, Yildirim-Toruner C, Oberle E, McDonald D, Sivaraman V, Ardoin S. Improving Lupus Care Index Documentation in Patients with Childhood-Onset Systemic Lupus Erythematosus (cSLE) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/improving-lupus-care-index-documentation-in-patients-with-childhood-onset-systemic-lupus-erythematosus-csle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-lupus-care-index-documentation-in-patients-with-childhood-onset-systemic-lupus-erythematosus-csle/