Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Lupus is an autoimmune disease primarily affecting women of reproductive age. Lupus confers an increased risk of adverse maternal fetal outcomes, and pre-pregnancy planning has been shown to improve pregnancy outcomes. We implemented a Quality Improvement (QI) initiative to improve contraceptive counseling rates in our female lupus patients of reproductive age.
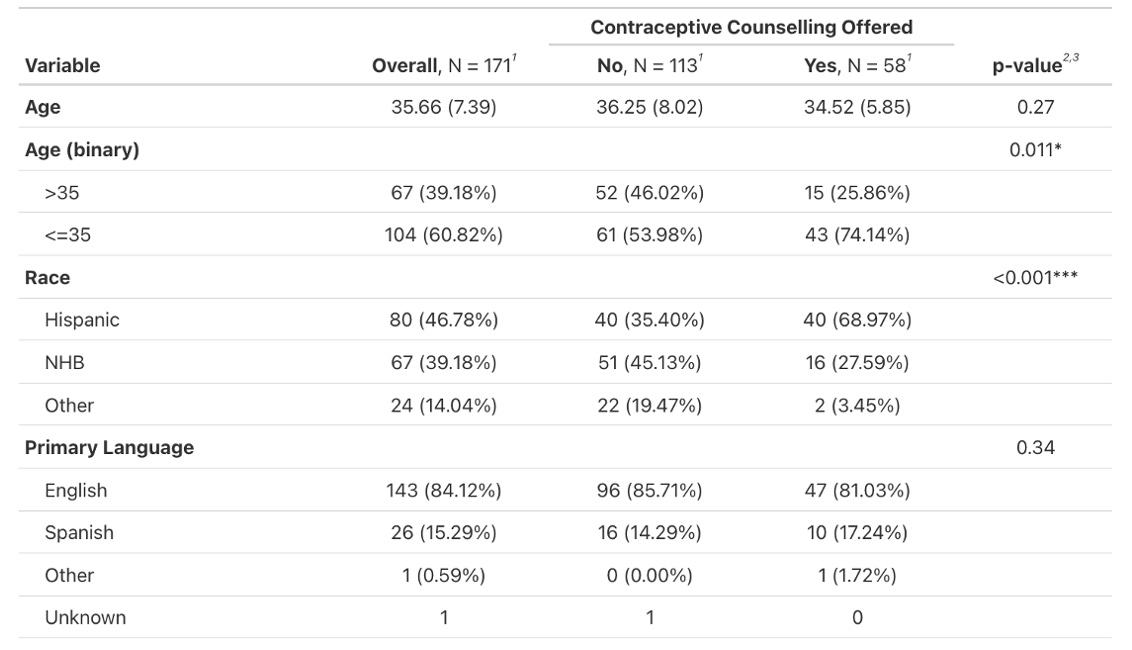
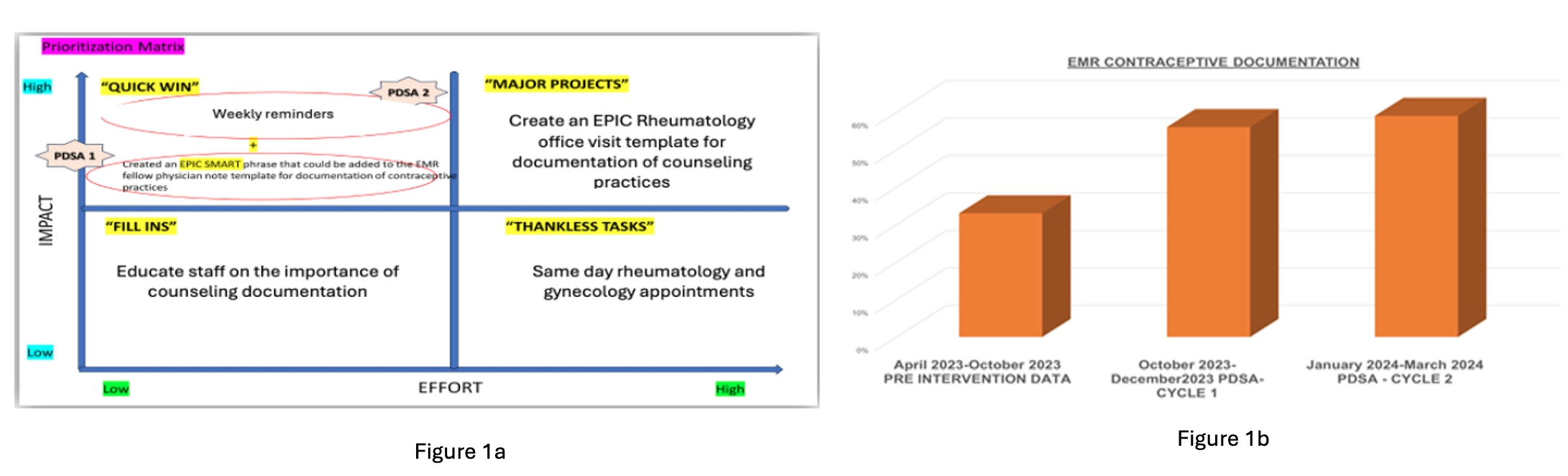
Methods: With Institutional Board Review approval, we queried electronic medical records for documentation of contraceptive counseling and demographic data of female lupus patients aged 15-50 years who visited the Montefiore Family Care Center (FCC) Lupus Clinic from April 2023 – April 2024. We assessed baseline contraception rates in our pre-intervention cohort from April 2023 – September 2023, then performed a QI initiative over the following 6 months. We utilized a QI process map to outline current counseling practices at FCC and identified barriers to counseling using survey data from rheumatology fellows. The primary barrier identified was the lack of a standardized EMR template for lupus office visits containing counseling reminders. We utilized a prioritization matrix to plan our intervention (Figure 1a) which included providing EMR templates to providers for clinic visits during our first plan-do-study-act (PDSA) cycle from October 2023 – December 2023. We added weekly reminders to perform contraceptive counseling for our second PDSA cycle from January 2024 – April 2024. Rates of contraceptive counseling were compared pre and post-intervention, with a subgroup analysis comparing counseling among women under or equal to 35 years versus women over 35 years (advanced maternal age). Statistical analysis was done using Chi-squared testing and logistic regression.
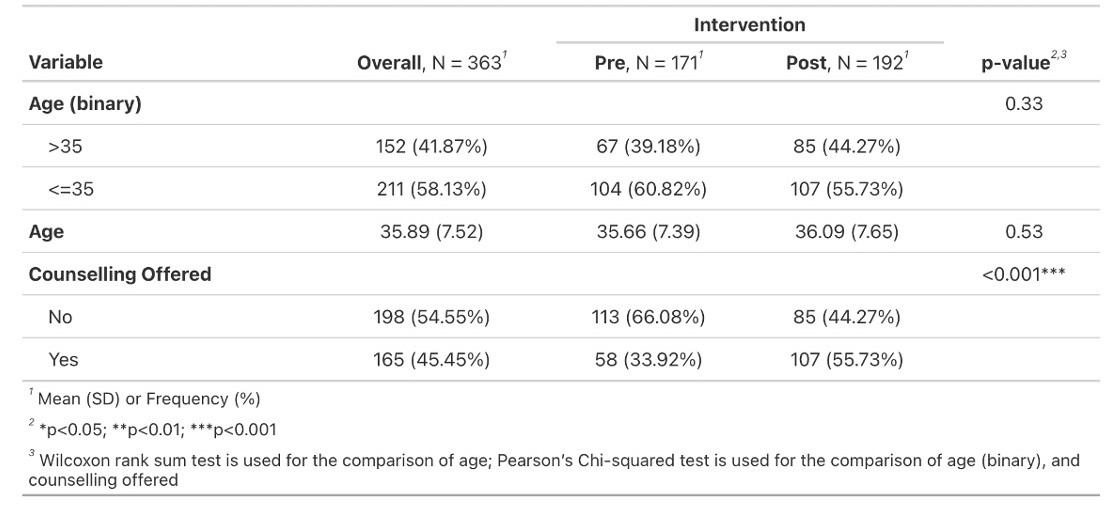
Results: Of the 171 clinic visits in the pre-intervention cohort, only 33.9% had contraceptive counseling documentation. Of those, women aged 35 and under were more likely to receive contraceptive counseling than those of advanced maternal age (p = 0.011) (Table 1). Non-Hispanic Black women were less likely to receive counseling than Hispanic women (p < 0.001). Of the 192 visits in the post-intervention cohort, 55.7% were offered contraceptive counseling (p < 0.001); the first PDSA cycle showed improvements in counseling rates to 56% and the second PDSA cycle improved rates to 59% (Figure 1b). Using logistic regression, post-intervention patients above age 35 were 4.09 times more likely to receive counseling compared to pre-intervention (p < 0.001) (Table 2).
Conclusion: Our results demonstrate a significant improvement in contraceptive counseling for female lupus patients, including those of advanced maternal age. This initiative can be replicated on a larger scale to minimize age disparities in lupus going forward.
To cite this abstract in AMA style:
Weisleder H, Osuorji C, Fazzari M, Jin Y, Ayesha B. Improving Age Disparities in Contraceptive Counseling in Women with Lupus: A Quality Improvement Initiative [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/improving-age-disparities-in-contraceptive-counseling-in-women-with-lupus-a-quality-improvement-initiative/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-age-disparities-in-contraceptive-counseling-in-women-with-lupus-a-quality-improvement-initiative/