Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Post-acute sequelae of COVID-19 (PASC) refers to persistent symptoms after the resolution of acute infection and is estimated to affect over 20% of COVID-19 survivors. Vaccination decreases the risk of severe acute outcomes but its impact on the etiology of PASC remains poorly understood. There are limited data on whether vaccination reduces PASC risk, especially in patients with systemic autoimmune rheumatic diseases (SARDs) where impaired responses to vaccines may leave those with breakthrough infection vulnerable to PASC.
Methods: We systematically identified SARDs patients with COVID-19 in a large multicenter academic healthcare system and invited all living patients to participate in a prospective cohort 28 days after their COVID-19 diagnosis. Patients completed surveys regarding demographics, SARD clinical characteristics, COVID-19 symptoms and their duration, and validated patient-reported outcome measures including pain, fatigue, and functional status. We defined PASC as any symptom lasting ≥ 28 days. We defined breakthrough infection as COVID-19 occurring ≥14 days after completion of the initial SARS-CoV-2 vaccine series (two doses of either the Moderna or Pfizer-BioNTech vaccines or one dose of the Johnson & Johnson-Janssen vaccine). Proportions of patients with PASC among those with and without breakthrough infection were compared using chi-square tests, and outcomes among those with PASC were compared between the two groups.
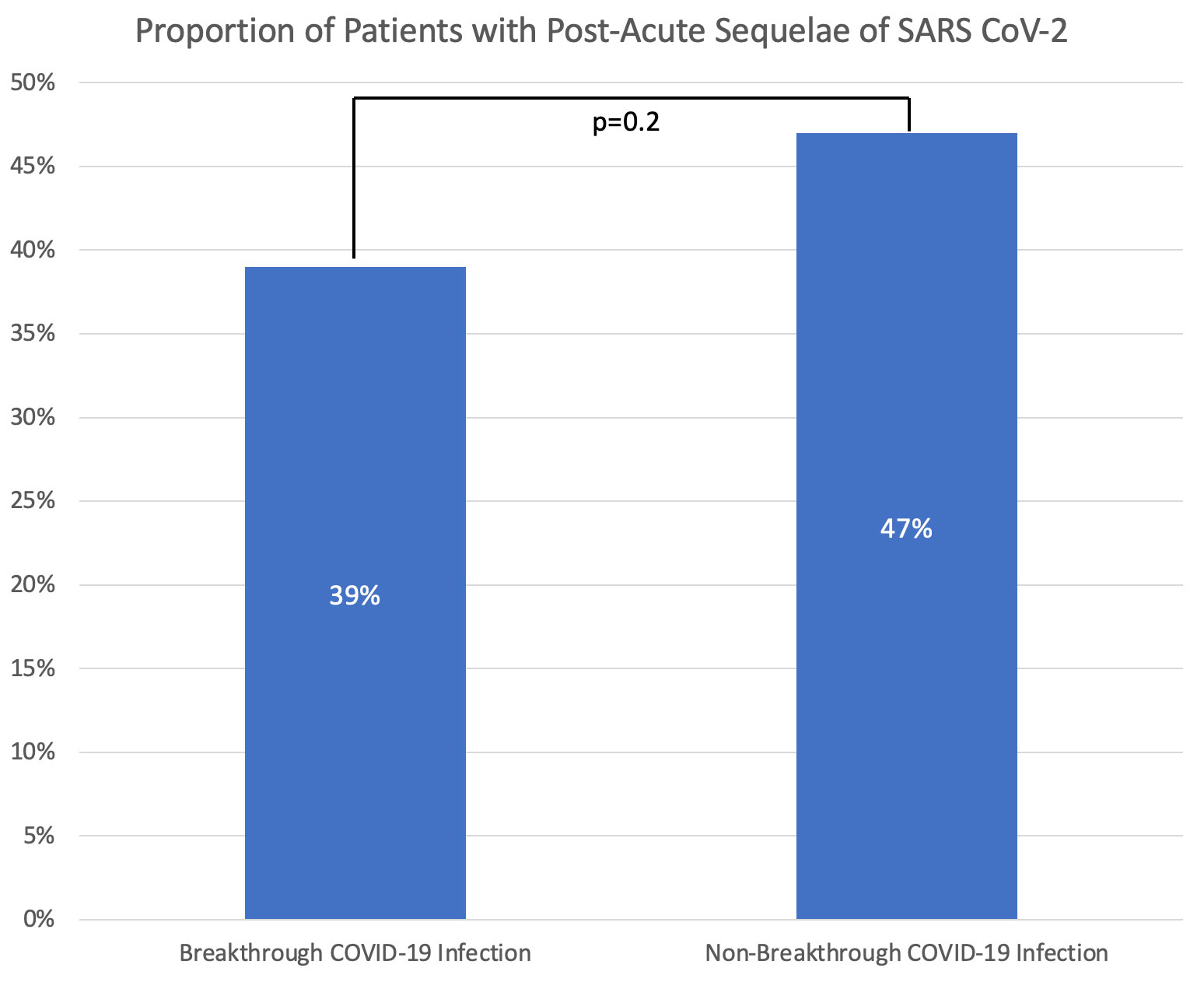
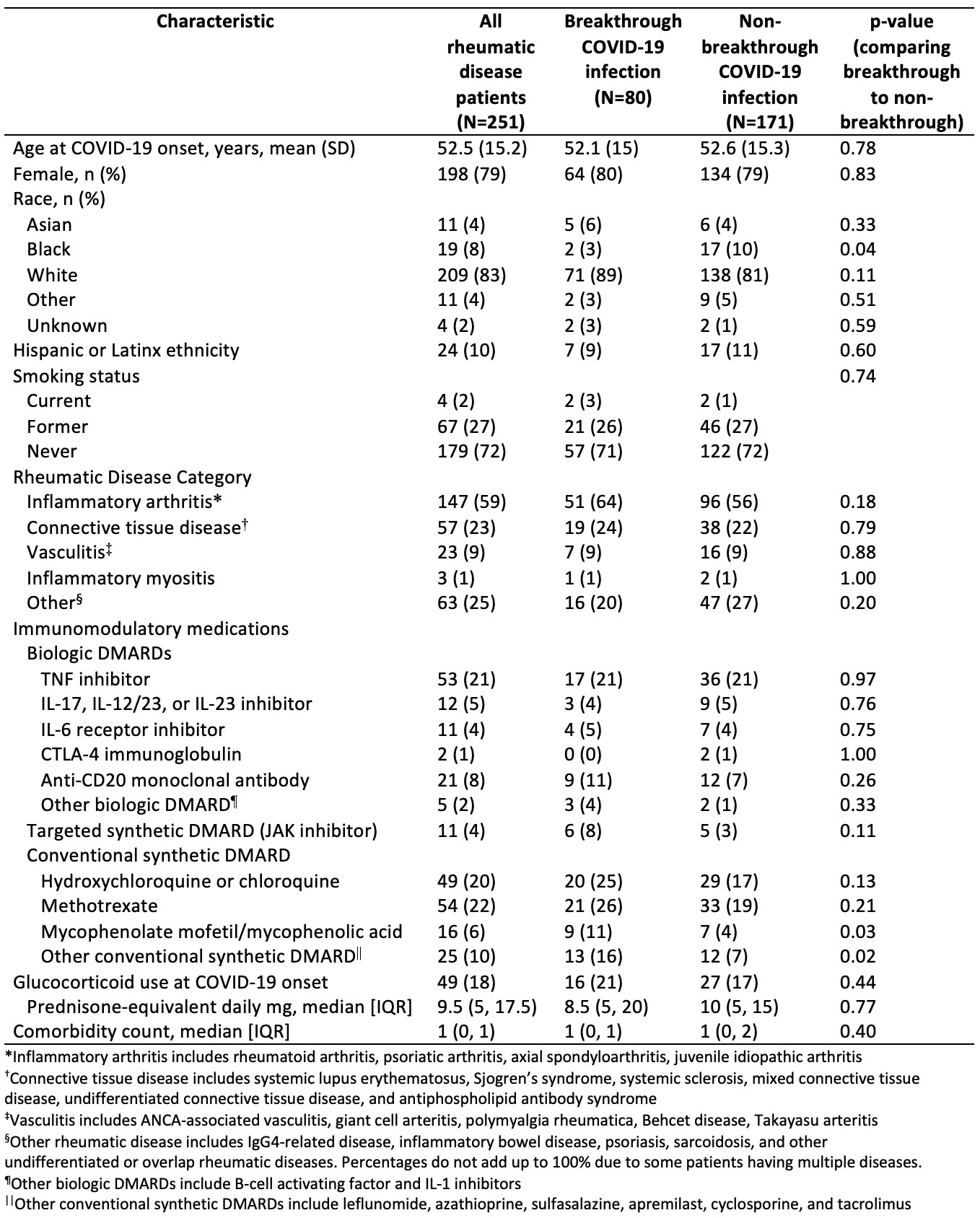
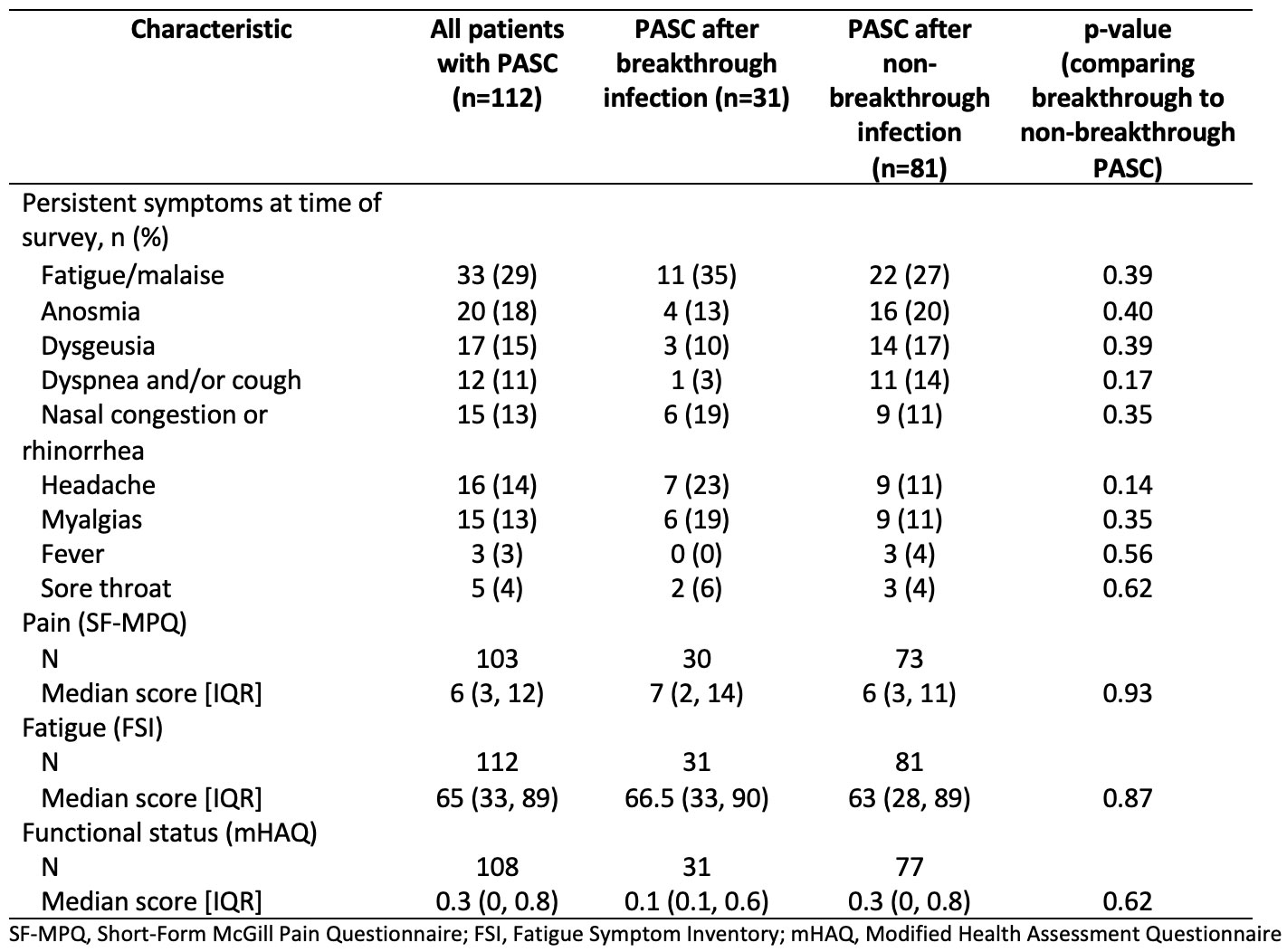
Results: Among 251 patients included in this analysis, the mean age was 53 years at COVID-19 diagnosis, 79.2% were female, and 83.3% were white (Table 1). The most common SARDs were rheumatoid arthritis (40.6%) and lupus (13.9%). The most common immunomodulatory medications were methotrexate (21.5%), TNF inhibitors (21.1%), and hydroxychloroquine (19.1%). The median (IQR) time from COVID-19 symptom onset to survey response was 191 days (94, 344). Fatigue was the most common symptom of acute COVID-19 (74.5%), followed by headache (58.6%) and fever (56.2%). The majority (86.0%) were not hospitalized. Compared to those without breakthrough infection, those with a breakthrough infection had numerically lower rates of PASC but this was not statistically significant (39% vs. 47%, p=0.2) (Figure). The most common persistent symptom was fatigue which was present in 29% of patients with PASC, followed by anosmia (18%) and dysgeusia (15%); there was a trend towards patients with breakthrough infection PASC more often having upper airway symptoms whereas non-breakthrough PASC more often had lower airway symptoms (Table 2). Pain, fatigue, and functional status scores were similar among those with PASC with and without breakthrough infection (Table 2).
Conclusion: Vaccinated patients with SARDs had numerically lower rates of PASC compared to those with no or partial prior vaccination. In addition to vaccination, our findings may also be related to differences in SARS-CoV-2 variants or acute COVID-19 treatments. Beyond reducing the severity of acute COVID-19 infection, ongoing strategies to improve vaccine uptake among SARD patients may have the additional benefit of reducing the risk of PASC.
To cite this abstract in AMA style:
Patel N, Kawano Y, Wang X, Fu X, Cook C, Vanni K, Qian G, Banasiak E, Kowalski E, zhang y, Sparks J, Wallace Z. Impact of Vaccination on Post-acute Sequelae of SARS CoV-2 Infection in Patients with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/impact-of-vaccination-on-post-acute-sequelae-of-sars-cov-2-infection-in-patients-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-vaccination-on-post-acute-sequelae-of-sars-cov-2-infection-in-patients-with-rheumatic-diseases/