Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Thrombocytopenia is associated with Systemic Lupus Erythematosus (SLE) and occurs at various stages of the disease. It is reported in an estimated 10% to 40% of patients. Previous studies to determine outcomes of thrombocytopenia in SLE patients have been small or single center. We therefore assessed the clinical significance of thrombocytopenia for SLE patients using a large national database which provides a representative sample of SLE patients admitted across the United States.
Methods: We identified patients who were hospitalized between January 1, 2020, and December 31, 2020, 18 years and older, from the National Inpatient Sample (NIS) database. The NIS is the largest publicly available all-payer inpatient care database in the United States. Patients with a diagnosis of SLE, with and without a concurrent diagnosis of thrombocytopenia were then identified using the International Classification of Diseases, Tenth Revision (ICD-10) codes. Our primary outcome was inpatient mortality, and secondary outcomes included length of stay (LOS) and total hospital charges. Multivariable logistic regression analysis was used to calculate the odds ratio for mortality adjusted for age, sex, race, Charlson comorbidity index, antiphospholipid syndrome (APS) and hemolytic anemia
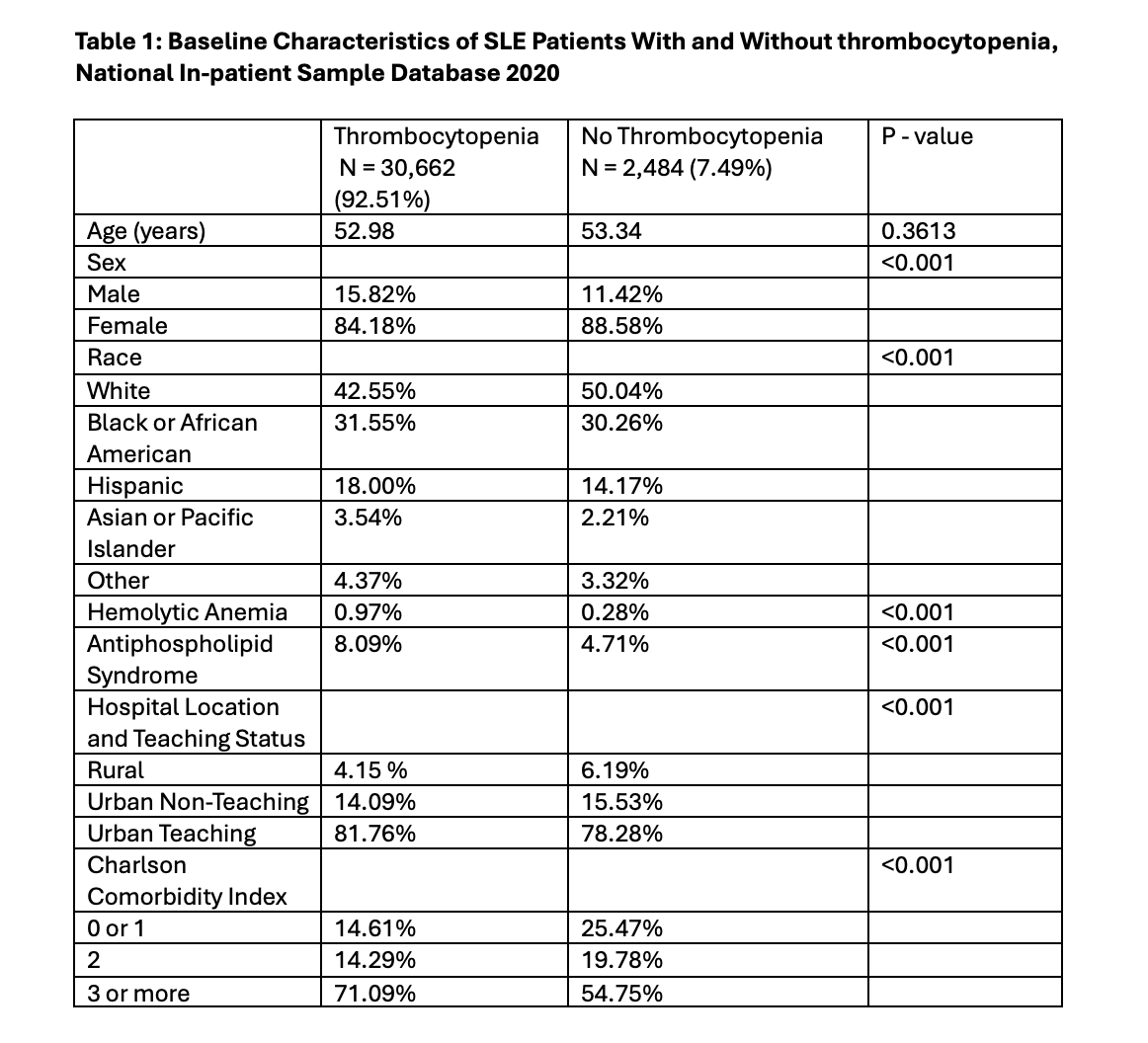
Results: A total of 33,146 patients with SLE were admitted over the study period, of which 2,484 (7.49%) had a diagnosis of thrombocytopenia. The mean age was similar in both groups (52.98 vs 53.34; p=0.3613). SLE patients with thrombocytopenia had a lower proportion of females (84.18% vs 88.58%; p=< 0.001) and a higher prevalence of hemolytic anemia (0.97% vs 0.28%; p = < 0.001) and APS (8.09% vs 4.71%; p= < 0.001) compared to those without thrombocytopenia. Patients with thrombocytopenia also had higher prevalence of multiple comorbidities as per Charlson comorbidity index (3 or more comorbidities 71.09% vs 54.75%; p=< 0.001) (Table 1).
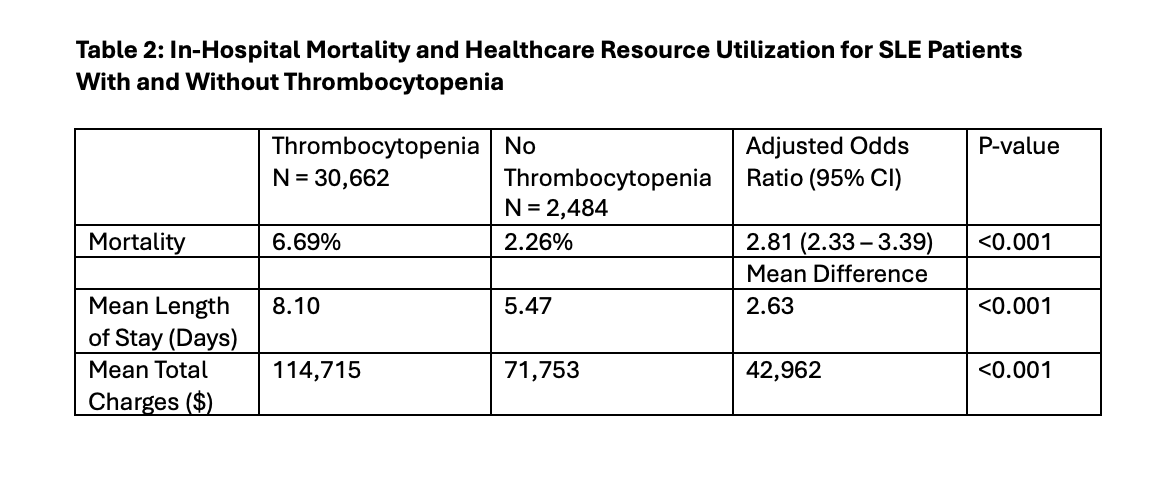
Inpatient mortality was significantly higher among SLE patients with thrombocytopenia [adjusted odds ratio (aOR) 2.81, 95% CI (2.33-3.39), p=< 0.001]. Thrombocytopenia was also associated with increased LOS and higher total charges with mean differences of 2.63 days and $42,962 respectively when compared to patients with no thrombocytopenia (Table 2).
Conclusion: This study demonstrated higher in-hospital mortality among SLE patients with thrombocytopenia, as well as higher healthcare resource utilization evidenced by increased LOS and higher total charges. SLE patients with thrombocytopenia may require closer inpatient monitoring and further studies are needed to investigate ways to improve outcomes for these patients.
To cite this abstract in AMA style:
Salia S, Mamoh U, Hedayati G, Atarere J, Wadie R, Mensah B, Morny J, Acharya I. Impact of Thrombocytopenia on In-hospital Mortality and Healthcare Resource Utilization in Patients with Systemic Lupus Erythematosus: An Analysis of the National Inpatient Sample Database 2020 [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-thrombocytopenia-on-in-hospital-mortality-and-healthcare-resource-utilization-in-patients-with-systemic-lupus-erythematosus-an-analysis-of-the-national-inpatient-sample-database-2020/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-thrombocytopenia-on-in-hospital-mortality-and-healthcare-resource-utilization-in-patients-with-systemic-lupus-erythematosus-an-analysis-of-the-national-inpatient-sample-database-2020/