Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: To determine whether remission and low disease activity state (LDAS) reduce hospitalizations in systemic lupus erythematosus (SLE) patients.
Methods: A multi-ethnic, multi-national Latin-American SLE cohort was studied.
Visits were performed every six months. Variables were ascertained at each visit. The first hospitalization following cohort entry was evaluated in the interval between two visits. Based on the definitions of remission in SLE (DORIS) framework, for each visit remission on treatment was defined as a SLEDAI of 0, prednisone ≤5 mg/day and maintenance treatment with immunosuppressants. LDAS was defined as a SLEDAI ≤4 with no SLEDAI scores for renal, central nervous system, serositis, vasculitis, and constitutional components, no increase in any SLEDAI component since the previous visit, and prednisone dose ≤7.5 mg/day. Immunosuppressants at maintenance doses were allowed for LDAS. Antimalarial treatment was allowed for both states. Potential confounders of hospitalization included sociodemographic factors, baseline damage (Systemic Lupus International Collaborating Clinics Damage Index or SDI), previous hospitalizations, glucocorticoids and antimalarials (users and non-users). Both, disease activity status and antimalarials were evaluated as time-dependent covariates. Cox regression model was used to evaluate whether remission on treatment and LDAS protected against hospitalizations after controlling for important confounders. A multivariable model was built by selecting covariates using a backward elimination procedure.
Results: One thousand three hundred and forty-one patients were included; 1201 (89.6%) were female. The median (IQR) age at diagnosis was 27 (20-37) years and the median (IQR) follow up time 27.5 (4.7-62.2) months. A total of 508 patients were hospitalized, of those 455 (89.6%) were female.
There were 6,089 intervals for these 1,341 patients. The median number of intervals per patient was 4 (2-7), and the median length of the intervals was 7.1 (5.1-11.7) months. Of the intervals examined, the most frequent status was non-optimally controlled, with 4,269 (75.1%) intervals, followed by remission on treatment 772 (13.6%) and LDAS 643 (11.3%) intervals. In the multivariable analysis, remission on treatment (HR 0.46; 95% CI 0.29–0.72) but not LDAS was found to decrease the hazard ratio of hospitalization, after adjusting for confounders. Of interest, antimalarials were found to be protective (HR: 0.61; 95% CI 0.51-0.72).
Conclusion: In this large Latin American multiethnic, multinational lupus cohort, remission on treatment reduced the risk of hospitalization after adjusting for other well-known risk factors. It is worth pointing out that antimalarial use seemed to protect against the occurrence of hospitalizations, supporting its role as a cornerstone treatment in SLE. Our findings call for seeking remission as a fundamental target in the management of patients with SLE.
Acknowledgments: The authors are grateful to Jennifer H Lofland, Federico Zazzetti, and Chetan Karyekar for their contributions.
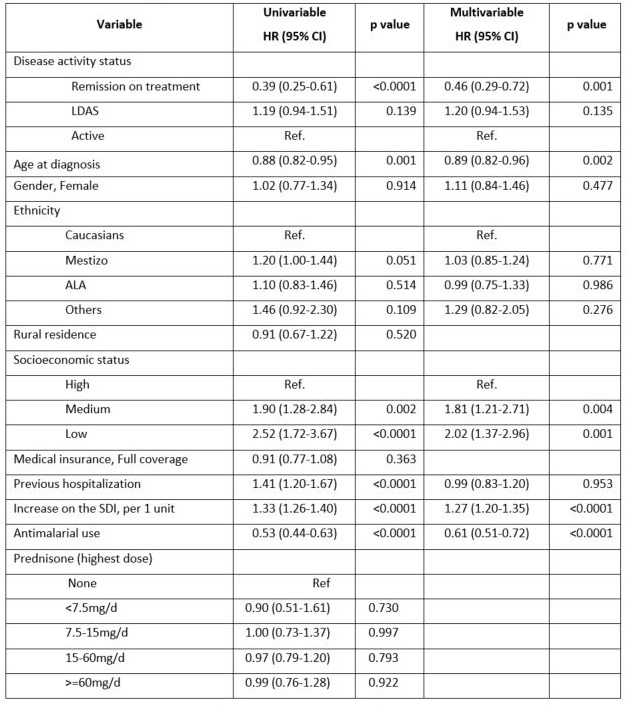 Table 1: Impact of disease activity status on hospitalization: univariable and multivariable analyses. LDAS: low disease activity status; ALA: Afro-Latin American; SDI: SLICC/ACR damage index; HR: Hazard ratio; 95% CI: 95% confidence interval; Ref: reference group
Table 1: Impact of disease activity status on hospitalization: univariable and multivariable analyses. LDAS: low disease activity status; ALA: Afro-Latin American; SDI: SLICC/ACR damage index; HR: Hazard ratio; 95% CI: 95% confidence interval; Ref: reference group
To cite this abstract in AMA style:
Pons-Estel G, Ugarte-Gil M, Harvey G, Wojdyla D, Quintana R, Serrano-Morales R, Gómez-Puerta J, García M, Catoggio L, Saurit V, Drenkard C, Da Silva N, Cavalcanti F, Borba E, Sato E, Neira O, Massardo L, Vásquez G, Alonso Gonzalez L, Guibert Toledan M, Silveira L, García De La Torre I, Sauza del Pozo M, Chacón R, Cardiel M, Alarcón G, Pons-Estel B. Impact of Remission and Low Disease Activity Status on Hospitalizations Among SLE Patients from the GLADEL Latin American Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/impact-of-remission-and-low-disease-activity-status-on-hospitalizations-among-sle-patients-from-the-gladel-latin-american-cohort/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-remission-and-low-disease-activity-status-on-hospitalizations-among-sle-patients-from-the-gladel-latin-american-cohort/
