Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Our prior qualitative work discovered a subgroup of patients with SLE who experience persistent symptoms of fatigue and widespread pain, even on self-described “good days.” The objective of this study was to utilize a modified version of the Systemic Lupus Activity Questionnaire (SLAQ) to identify this subgroup of patients and measure the impact of this high symptom burden on health-related quality of life (HRQoL).
Methods: SLE patients meeting SLICC criteria were enrolled in lupus registry at a tertiary care center. Rheumatologists completed the SLEDAI and Physician Global Assessment (PGA). Active SLE was defined as SLEDAI ≥6, clinical SLEDAI ≥4, PGA ≥1, or active nephritis. Patients completed the Polysymptomatic Distress Scale and LupusPRO. We adapted the SLAQ to ask, “Thinking of your most recent good day with lupus, please rate the activity of your lupus,” with a scale of 0 (no lupus activity) to 10 (most lupus activity). We also asked patients’ frequency of good days (never, seldom, some of the time, or most of the time). Patients were grouped based on their score as having a “Good” good day (scores of 0 to 4) or “Bad” good day (scores of 5-10). Descriptive statistics estimated differences between groups.
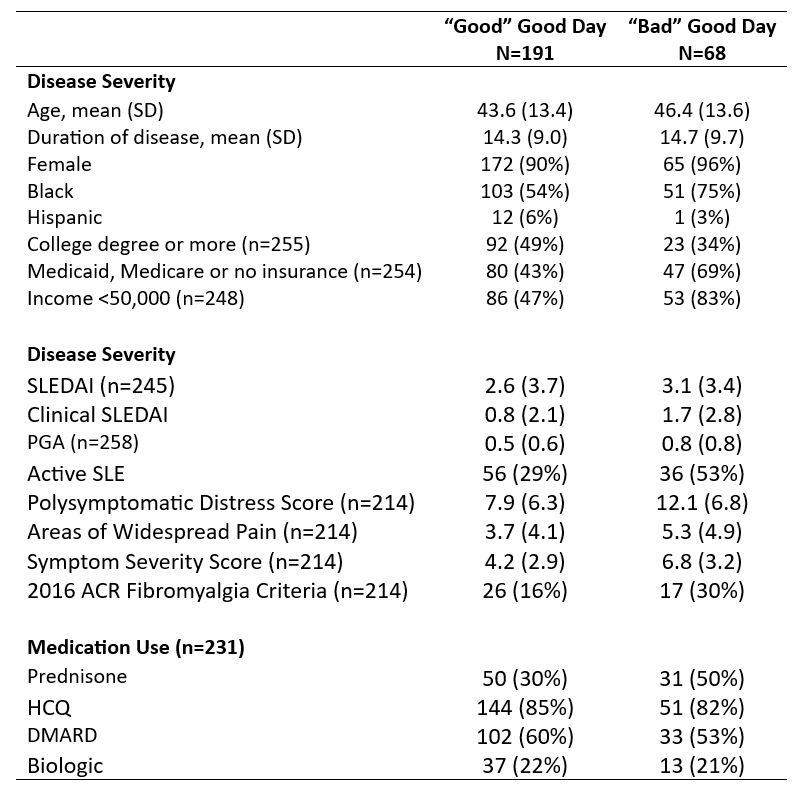
Results: The survey was completed by 259 patients (mean age 44 years, 92% female, 59% Black, 5% Hispanic). A “Good” good day was reported by 74% of patients, while 26% of patients reported a “Bad” good day. Patients with “Bad” good days were more likely to have an annual income less than $50,000, have education less than a college degree, and be insured through Medicaid or Medicare or be uninsured; otherwise, demographics were similar (Table 1). Patients with “Bad” good days had higher clinical SLEDAI and PGA scores, with 53% having active SLE at the time of their visit, compared to 29% of patients with “Good” good days. Patients with “Bad” good days experienced more polysymptomatic distress, and 30% met ACR criteria for fibromyalgia, compared to 16% of patients with “Good” good days.
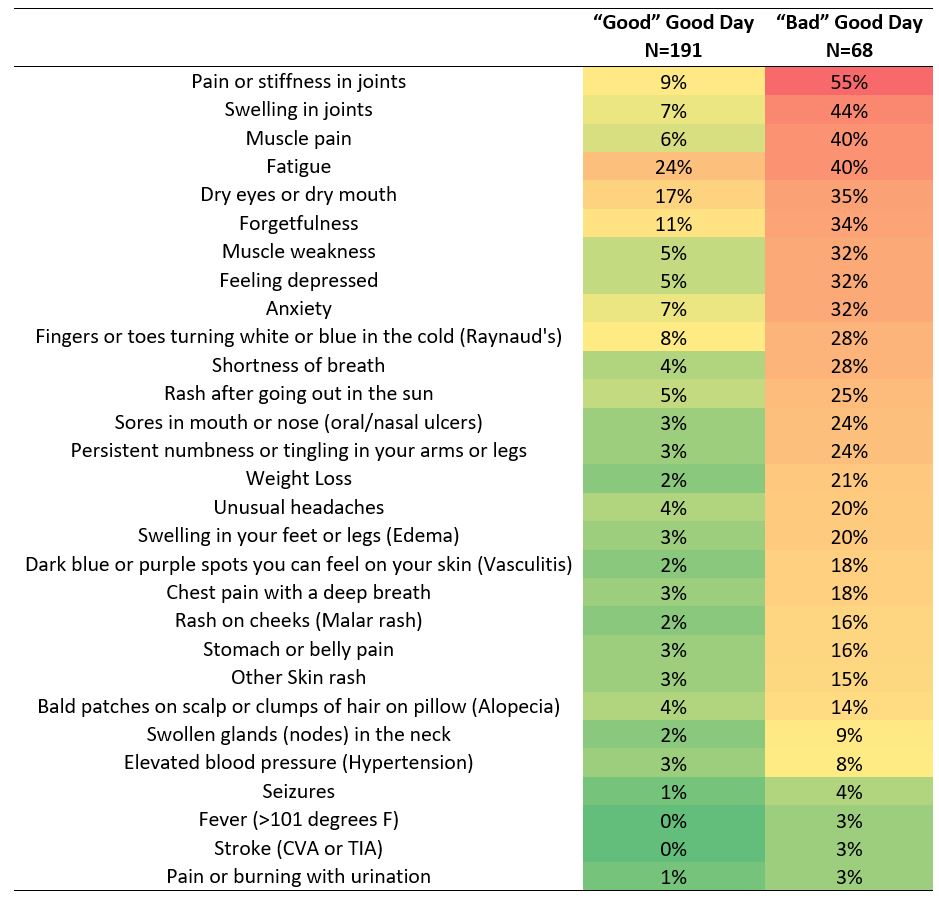
Most patients with “Good” good days were asymptomatic (Table 2), and 93% experienced good days most or some of the time. Even so, 24% experienced moderate to severe fatigue on their good days. In contrast, patients with “Bad” good days experienced moderate to severe symptoms of pain or stiffness in joints, swelling in joints, muscle pain, fatigue, forgetfulness, muscle weakness, depression, and anxiety. In this group of patients, good days were less frequent, with 26% saying they seldom or never had a good day.
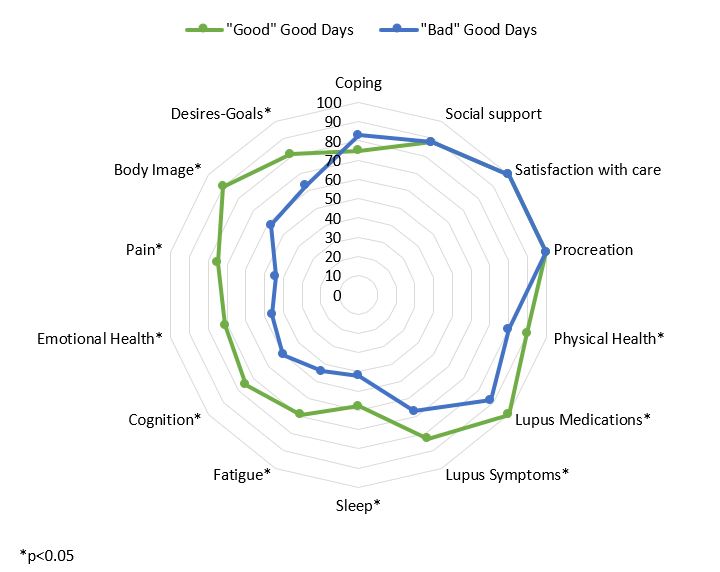
Patients with “Bad” good days experienced decreased HRQoL, with worse LupusPRO domain scores for lupus symptoms, cognition, lupus medications, physical health, sleep, fatigue, pain, emotional health, body image, and desires, goals, and plans (Figure 1).
Conclusion: There is a subset of patients with SLE who experience symptoms of pain and fatigue even on their self-described good days. This burden of symptoms has a significant impact on patients’ quality of life. While almost one-third of patients with the highest burden of symptoms met ACR criteria for fibromyalgia, half of patients also had active inflammatory SLE symptoms on the day of the visit, suggesting isolated fibromyalgia is not the only contributor to poor quality of life in patients with SLE.
To cite this abstract in AMA style:
Eudy A, Clowse M, Jolly M, Pisetsky D, Sun K, Sadun R, Criscione-Schreiber L, Maheswaranathan M, Doss J, Rogers J. Impact of Pain and Fatigue on Quality of Life Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-pain-and-fatigue-on-quality-of-life-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-pain-and-fatigue-on-quality-of-life-among-patients-with-systemic-lupus-erythematosus/