Session Information
Date: Tuesday, November 15, 2016
Title: Spondylarthropathies and Psoriatic Arthritis – Clinical Aspects and Treatment - Poster III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Studies have shown that psoriasis of the skin, scalp and/or nails precedes the appearance of psoriatic arthritis (PsA) by up to 12 years1,2; however, only a single European study from a German registry has examined PsA patients with nail psoriasis in clinical practice.3 The objective of this descriptive analysis was to characterize the clinical and patient-reported outcomes of PsA patients with nail psoriasis in the US-based Corrona Psoriatic Arthritis/Spondyloarthritis (PsA/SpA) registry.
Methods: This cross-sectional descriptive study included all patients enrolled in the Corrona PsA/SpA registry between March 2013 and March 2016 with a diagnosis of PsA who had non-missing data on physician-reported nail psoriasis. Patients were stratified by presence vs absence of nail psoriasis, defined as having a non-zero response on the nail psoriasis visual analog scale of 0–100. Descriptive analyses of patient demographics, clinical measures, patient-reported outcomes and treatment characteristics were assessed at the time of enrollment and compared between subgroups using P values from Wilcoxon rank-sum tests for continuous variables and chi-squared tests for categorical variables.
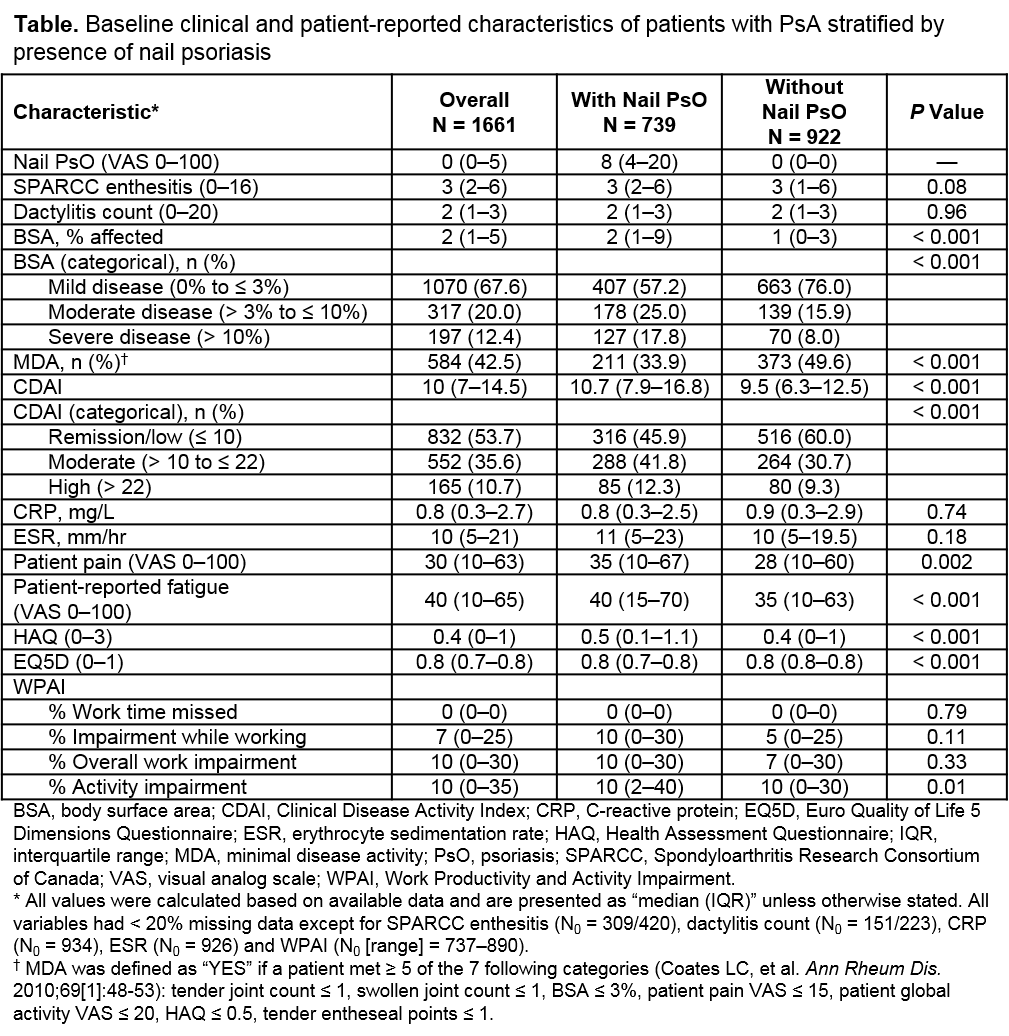
Results: As of March 2016, a total of 1661 patients with PsA in the registry met the inclusion criteria, including 739 patients (44.5%) with nail psoriasis and 922 patients (55.5%) without nail psoriasis. Both patient subgroups were similar in terms of age, race, body mass index, disease duration, prevalence of most comorbidities (e.g., cardiovascular disease, any cancer, diabetes and serious infection) and biologic use at the time of enrollment; however, patients with nail psoriasis were significantly more likely to be male (53.0% vs 43.8%) and have a higher history of depression (35.9% vs 27.4%), and were less likely to be underweight/normal (13.1% vs 19.0%) compared with patients without nail psoriasis. Patients with nail psoriasis had more moderate/severe psoriasis at enrollment (body surface area [BSA] > 3%) compared with patients without nail psoriasis, and had worse disease as assessed by percentage of affected BSA, achievement of minimal disease activity, Clinical Disease Activity Index scores, physical function, patient-reported pain and fatigue, quality of life and activity impairment (Table).
Conclusion: This analysis from the Corrona registry demonstrated that patients with PsA and nail psoriasis at the time of registry enrollment had significantly worse disease activity and had worse patient-reported outcomes compared with those patients without nail involvement. Nail psoriasis is common in patients with PsA; therefore, these findings emphasize the importance of early recognition and management of patients with nail psoriasis.
References:
1. Nestle FO, et al. N Engl J Med. 2009;361(5):496-509.
2. Boehncke WH, et al. Br J Dermatol. 2014;170(4):772-86.
3. Langenbruch A, et al. Br J Dermatol. 2014;171(5):1123-8.
To cite this abstract in AMA style:
Mease PJ, Palmer JB, Litman HJ, Karki C, Greenberg JD. Impact of Nail Psoriasis on Clinical Presentation of Psoriatic Arthritis—Descriptive Analysis from the Corrona Psoriatic Arthritis/Spondyloarthritis (PsA/SpA) Registry [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/impact-of-nail-psoriasis-on-clinical-presentation-of-psoriatic-arthritis-descriptive-analysis-from-the-corrona-psoriatic-arthritisspondyloarthritis-psaspa-registry/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-nail-psoriasis-on-clinical-presentation-of-psoriatic-arthritis-descriptive-analysis-from-the-corrona-psoriatic-arthritisspondyloarthritis-psaspa-registry/