Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite significant interest in using health information technology (IT) to improve processes of care such as documentation of disease activity in RA, few studies have evaluated the impact of process improvements on actual health outcomes. In this study, we assessed whether 2 health-IT initiatives that improved collection and documentation of RA disease activity scores in a large academic rheumatology clinic resulted in concomitant improvements in clinical outcomes over time.
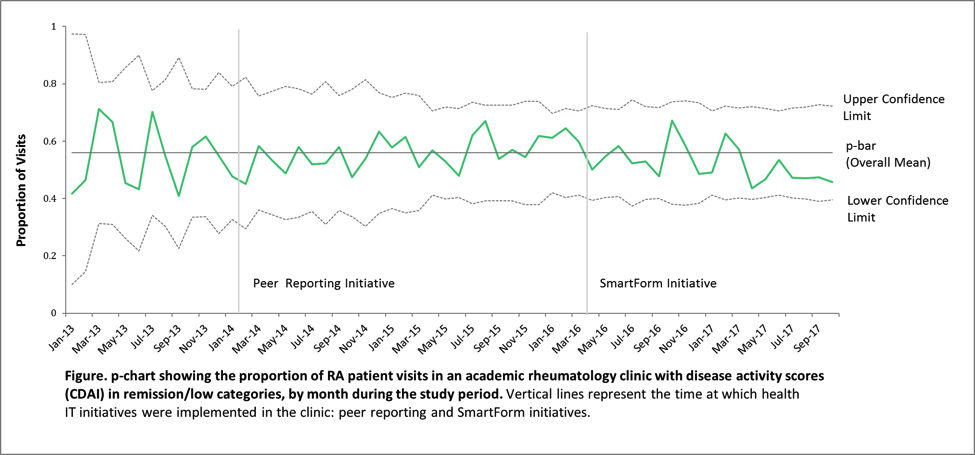
Methods: We examined 2 initiatives designed to facilitate Clinical Disease Activity Index (CDAI) documentation: 1) a monthly peer report of physicianÕs performance on CDAI documentation, and 2) introduction of an electronic health record (EHR) SmartForm with an embedded CDAI calculator to make collection and tracking of disease activity scores more efficient. All adult RA patients with ³ 2 encounters in our rheumatology clinic with ³ 1 CDAI documented (64% of all RA encounters) between 1/2013 – 10/2017 were included. Data derived from our EHR data warehouse included demographics, encounter dates, and CDAI scores. We compared mean CDAI 12 months pre- and post- the peer reporting initiative and 19 months pre- and post- the SmartForm initiative with t-tests. Paired t-tests were performed on a subgroup of patients with ³ 1 CDAI pre- and post- each initiative to assess whether there was significant change in CDAI over time for the same patient. The proportion of visits with a low/remission CDAI (CDAI²10) each month were examined using a control chart.
Results: We included 920 RA patients with 7171 encounters over 5 years. 82% were female; mean age was 57±16, 50% identified as non-White, and 13% preferred a language other than English (e.g. Chinese or Spanish). Mean CDAI was stable pre- and post- the peer reporting initiative (12.4) and increased slightly after the SmartForm initiative (from 11.3 to 13.4, p<0.05). Paired t-test detected small disease activity improvements after the peer reporting initiative (n=237, mean CDAI from 12.0 to 10.7, p<0.05) but worse scores after the SmartForm initiative (n=341, mean CDAI from 11.2 to 12.7, p<0.05). Though these changes were statistically significant, they did not exceed the minimally clinically important difference thresholds for CDAI. The overall proportion of visits with a CDAI in the low/remission category increased from 42 to 46% during the study period (Figure).
Conclusion: Although 2 quality improvement initiatives resulted in sustained improvements in disease activity score documentation, we did not see parallel gains in actual CDAI scores. These findings demonstrate that recording CDAI scores is not sufficient to improve disease activity without a comprehensive treat-to-target program. Additional efforts are underway in our health system to build a health-IT intervention to support providers and patients in improving RA outcomes.
To cite this abstract in AMA style:
Li J, Gandrup J, Trupin L, Izadi Z, Yazdany J, Schmajuk G. Impact of Gains in Rheumatoid Arthritis Disease Activity Documentation on Outcomes over Time [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/impact-of-gains-in-rheumatoid-arthritis-disease-activity-documentation-on-outcomes-over-time/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-gains-in-rheumatoid-arthritis-disease-activity-documentation-on-outcomes-over-time/