Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Risk of end stage renal disease (ESRD) is increased in patients with systemic lupus erythematosus (SLE). Due to lifestyle –related risk factors, inflammation, and medications such as steroids, SLE patients are also more likely to have diabetes mellitus (DM), the leading cause of ESRD in the world. We estimated the impact of DM on ESRD incidence in a large inception cohort of patients with SLE.
Methods: All adult patients registered with SLE International Classification of Diseases (ICD) codes in the Danish National Patient Register (DNPR) from January 1, 1996 to July 31, 2018 were identified. Individuals had no SLE ICD codes prior to 1996 (incident cases, n=3178). The date of this first SLE registration was set as SLE diagnosis date (baseline). DM was defined as the date of first DM ICD code or the date of first filled DM prescription (National Register of Medicinal Product Statistics). ESRD was defined as first registration of dialysis, renal transplant or terminal (stage 5) kidney insufficiency using ICD codes. Patients with prevalent ESRD at baseline were excluded from the analyses (n=29). ESRD incidence was compared in those with DM vs those without DM (non-DM). Incidence rates per 1000 person years (IRs) and incidence rate ratios (IRRs) with corresponding 95% confidence intervals (95% CI) were estimated, stratified by gender, age at baseline (< 50 years vs >= 50 years) and educational level at baseline. Poisson regression estimated IRR.
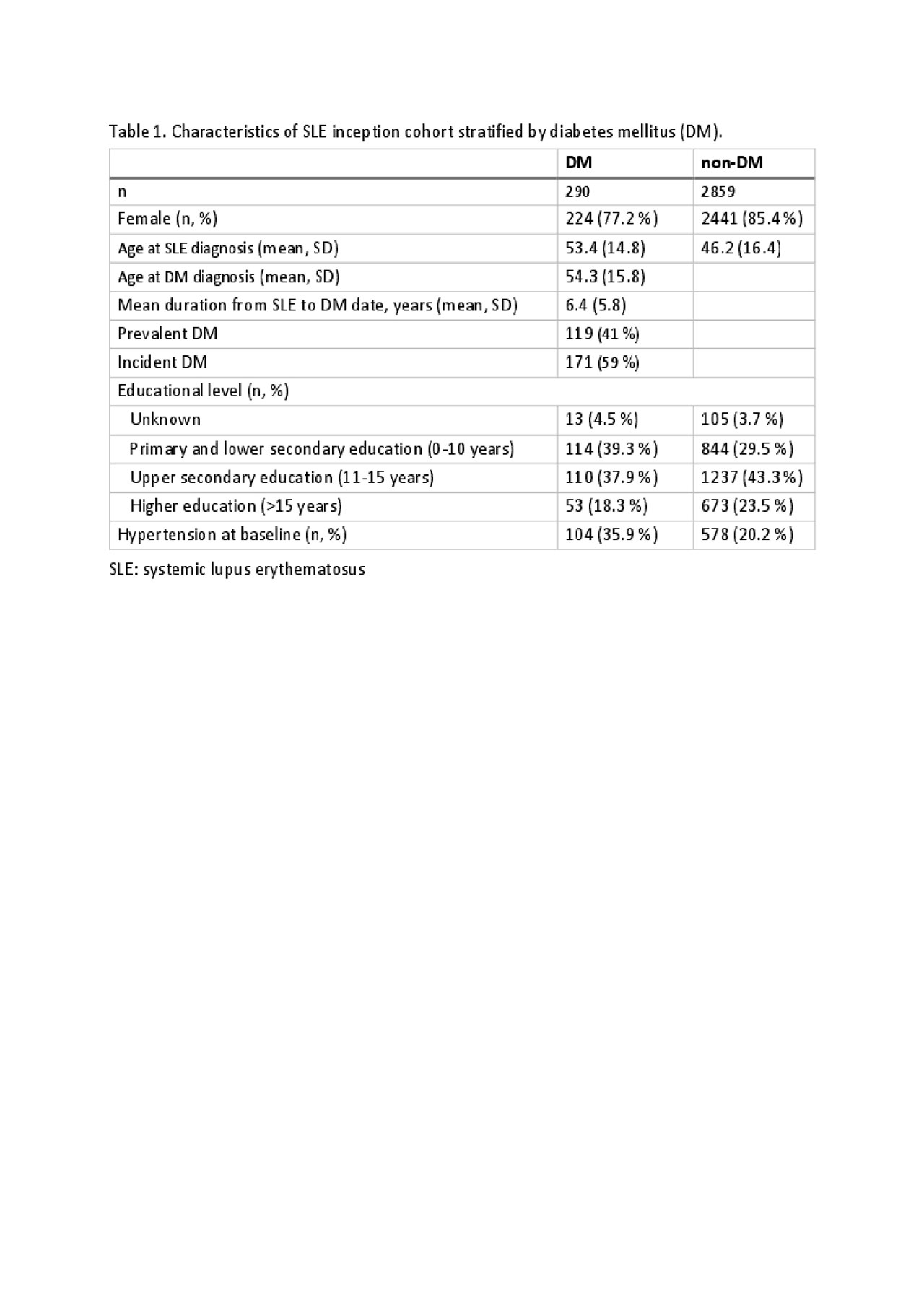
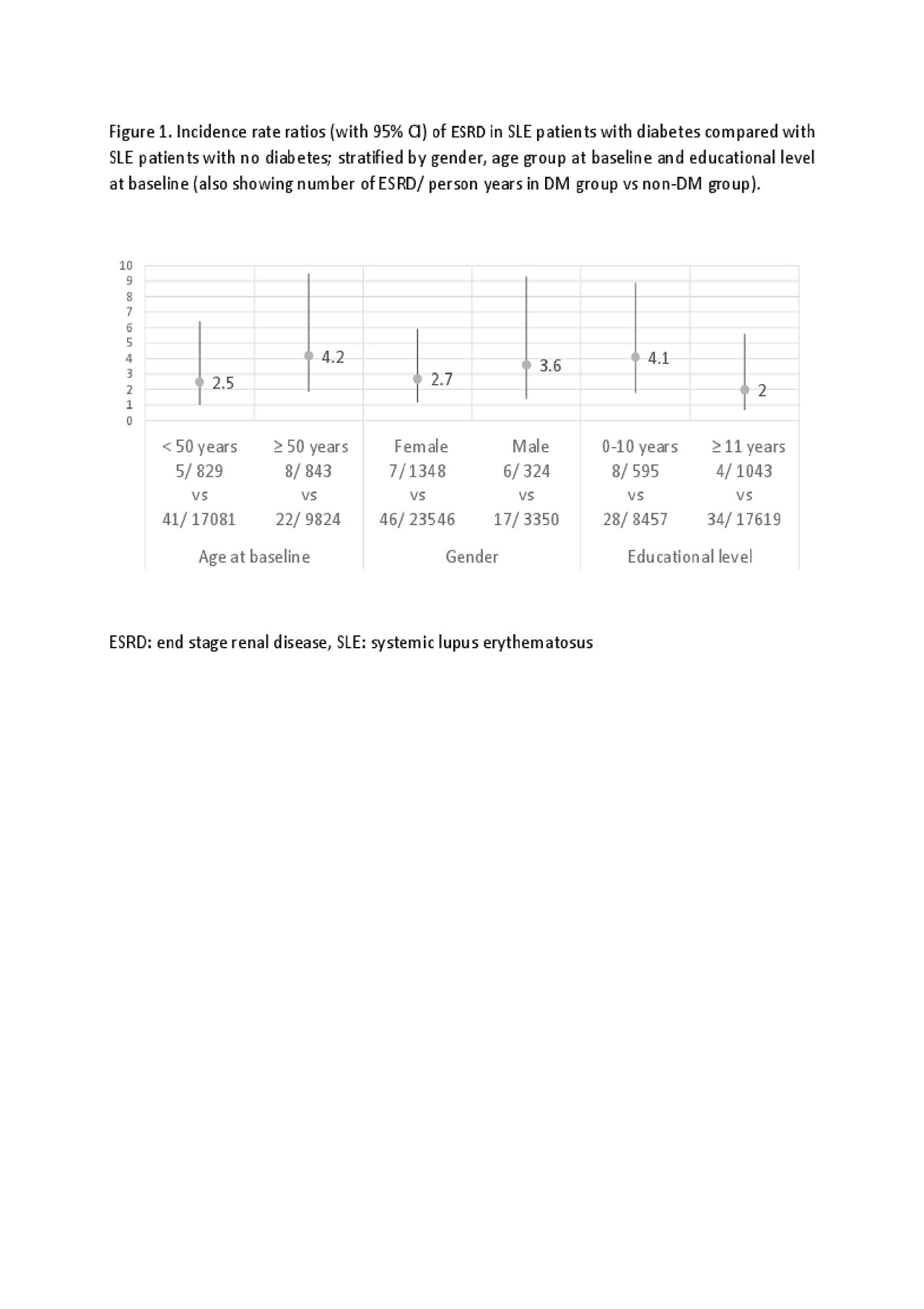
Results: The DM group included 290 patients of whom 77% were female compared to 85% of the 2859 in the non-DM group. Those with DM were older at baseline (53 vs 46 years) (Table 1). Of those with DM at any time, DM was prevalent at baseline in 119 (41%) and incident in 171 (59%) of the patients. Mean duration from SLE to DM date for patients with incident DM was 6.4 years. Hypertension was more prevalent at baseline in those with DM compared with the non-DM group (35 % vs 20 %). Patients with DM had nearly 3 times higher incidence rate of ESRD compared with non-DM patients, adjusted for gender, age, and educational level (2.6 (1.4-4.9)). The rates were higher in females, patients aged ≥50 years, and those with lower educational level (Figure1). However, due to overlapping CIs these differences might not be significantly different from one another.
Conclusion: We found that DM greatly increased the risk of ESRD in SLE patients. Timely diagnosis and treatment of comorbidities like DM are essential to prevent long term complications and damage accrual in SLE patients.
To cite this abstract in AMA style:
Hansen R, Simard J, Faurschou M, Jacobsen S, Falasinnu T. Impact of Diabetes on Risk of End Stage Renal Disease in Danish Nationwide Cohort of Newly Diagnosed Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-of-diabetes-on-risk-of-end-stage-renal-disease-in-danish-nationwide-cohort-of-newly-diagnosed-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-diabetes-on-risk-of-end-stage-renal-disease-in-danish-nationwide-cohort-of-newly-diagnosed-patients-with-systemic-lupus-erythematosus/