Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Studies have suggested that the chronic inflammatory nature of rheumatic conditions (rheumatoid arthritis (RA) and psoriatic arthritis (PsA)) as well as psoriasis (PsO) may predispose patients to cardiovascular (CV) disease and metabolic disorders. However, the individual impact of RA, PsA, PsO, and their treatments, on traditional CV risk factors – hypertension, diabetes mellitus (DM), hyperlipidemia, and obesity – is not well understood.
Methods: Patients with RA, PsA, and PsO with visits between January 1, 2002 and June 30, 2014 were identified (and included in three separate cohorts) in MarketScan, a large US employer-based claims database. The index date was defined as the date of RA, PsA or PsO diagnosis, and patients were required to be continuously enrolled for 12 months prior to the index date. Four cohorts were defined for each of the three diagnoses based on treatment (or lack thereof) during follow-up. The four cohorts were 1) TNF inhibitor (TNFi) monotherapy, 2) non-biologic (nb)DMARD monotherapy, 3) TNFi + any other nbDMARD combination therapy, and 4) No DMARD treatment. The treatment cohorts were followed from the date treatment was initiated after the index date until disenrollment, end of study period, switching medications to qualify for a different treatment cohort, or until the last available day supply of any medication in the designated treatment cohort. The primary outcome was the first occurrence of the CV risk factors during the follow-up period. Incidence rates (IR) per 1,000 patient-years (PY) with 95% confidence intervals (CI) were calculated. Incidence outcomes were age- and sex-standardized to the MarketScan general population.
Results: We identified 126,820 patients with RA, 18,924 with PsA, and 28,788 with PsO. Mean age at index date was similar for both PsO and PsA patients (50 yrs), but RA patients were older (56 yrs). Mean follow-up time ranged from 2.4 years to 3.0 years. Among RA patients, incidence rates of the 4 CV outcomes were fairly consistent between DMARD treated and non-treated patients, with numerically lower rates for hyperlipidemia and obesity. In PsO patients, monotherapy cohorts had higher rates of all outcomes than those not receiving any DMARDs. In PsA patients, rates of hypertension, diabetes and obesity were similar among all treatment groups, whereas hyperlipidemia displayed numerically higher rates among the DMARD treated cohorts (Table 1).
Conclusion: Impact of treatment on CV risk factors is not consistent across disease states or the CV risk factors. When treating patients there needs to be consideration for both the underlying disease states, and the CV risk factor of interest. The results highlight the importance of close monitoring and careful management of CV risk factors in patients with RA, PsA and PsO. 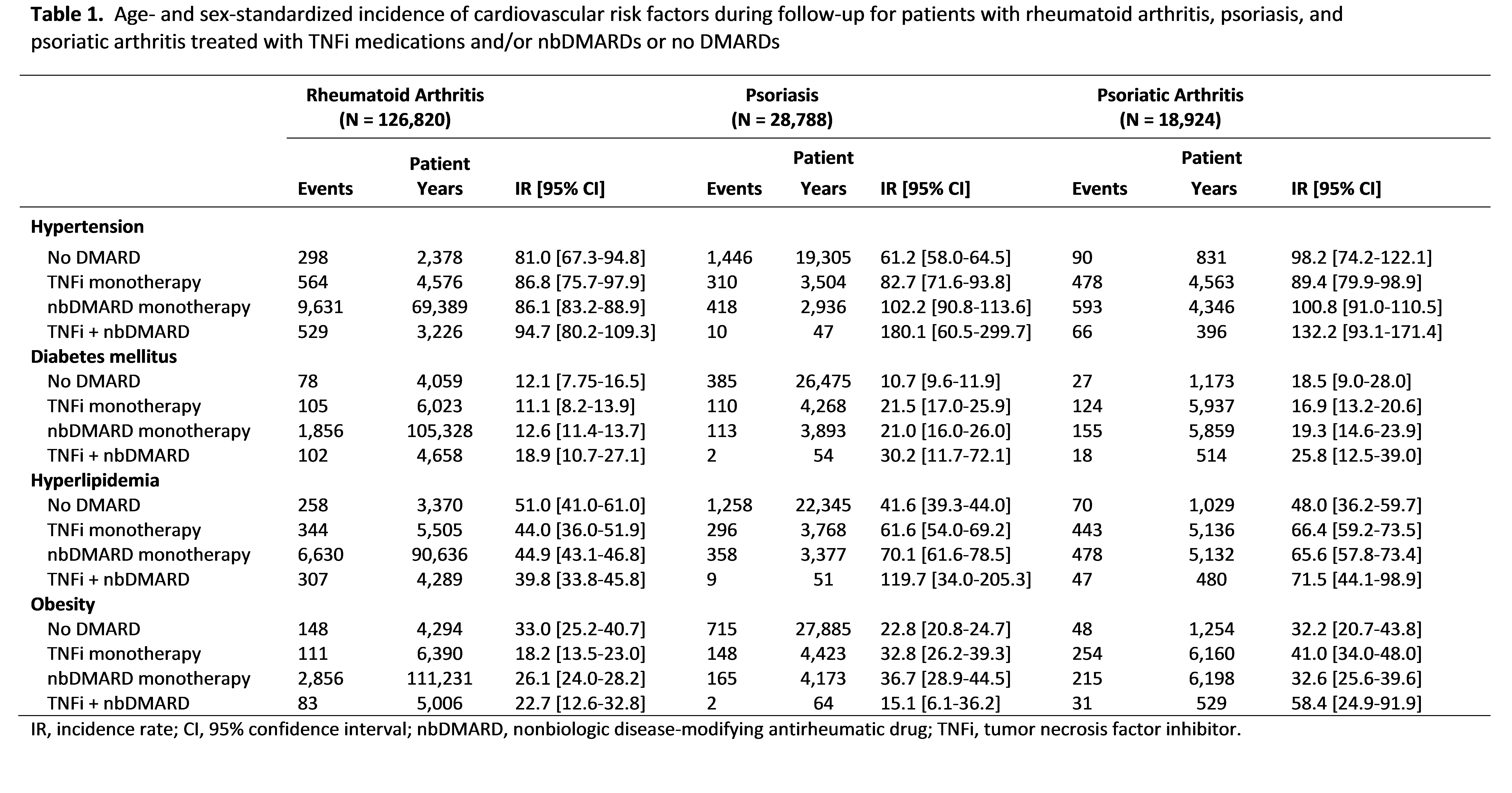
To cite this abstract in AMA style:
Radner H, Lesperance T, Accortt NA, Solomon DH. Impact of Biologic and Non-Biologic Treatment on the Incidence of Traditional Cardiovascular Risk Factors Among Patients with Rheumatoid Arthritis, Psoriatic Arthritis, or Psoriasis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/impact-of-biologic-and-non-biologic-treatment-on-the-incidence-of-traditional-cardiovascular-risk-factors-among-patients-with-rheumatoid-arthritis-psoriatic-arthritis-or-psoriasis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-biologic-and-non-biologic-treatment-on-the-incidence-of-traditional-cardiovascular-risk-factors-among-patients-with-rheumatoid-arthritis-psoriatic-arthritis-or-psoriasis/
