Session Information
Session Type: Abstract Session
Session Time: 10:45AM-11:00AM
Background/Purpose: AIIRD patients may have a blunted immune response to the COVID-19 vaccines, but this is largely uncharacterized as these individuals were not included in clinical trials. Vaccine response may be affected by patients’ underlying disease processes and the systemic immunomodulatory therapies used to treat them, although the evidence for this is uncertain. To better understand the immunogenicity of the COVID-19 vaccines in this patient population and their treatment regimens, we quantified humoral responses to the SARS-CoV-2 spike protein in AIIRD patients.
Methods: This exploratory, descriptive, prospective cohort study enrolled patients from a single-specialty practice in Charlotte, NC who received the BNT162b2 (Pfizer), mRNA-1273 (Moderna) or Ad26COV2.S (Johnson & Johnson) vaccine from 3/17/21-5/14/21. Those with prior COVID-19 by self-report were excluded. We collected demographics, AIIRD diagnoses and immunomodulatory regimens of these patients. Antibody (Ab) testing was performed at least 14 days after completion of their vaccine series. SARS-CoV-2 IgG Ab levels to the S1 spike antigen RBD were measured using a semi-quantitative assay (Siemens Atellica; Quest). Associations between clinical characteristics and Ab responses were evaluated.
Results: Characteristics of 291 AIIRD patients studied are listed in Table 1. Overall, 71% developed an Ab response with a mean Ab titer of 12.72 (< 1 index). There was no difference based on gender. The likelihood of an absent Ab response increased with age, and there was a decline in mean levels with aging in Ab+ patients.
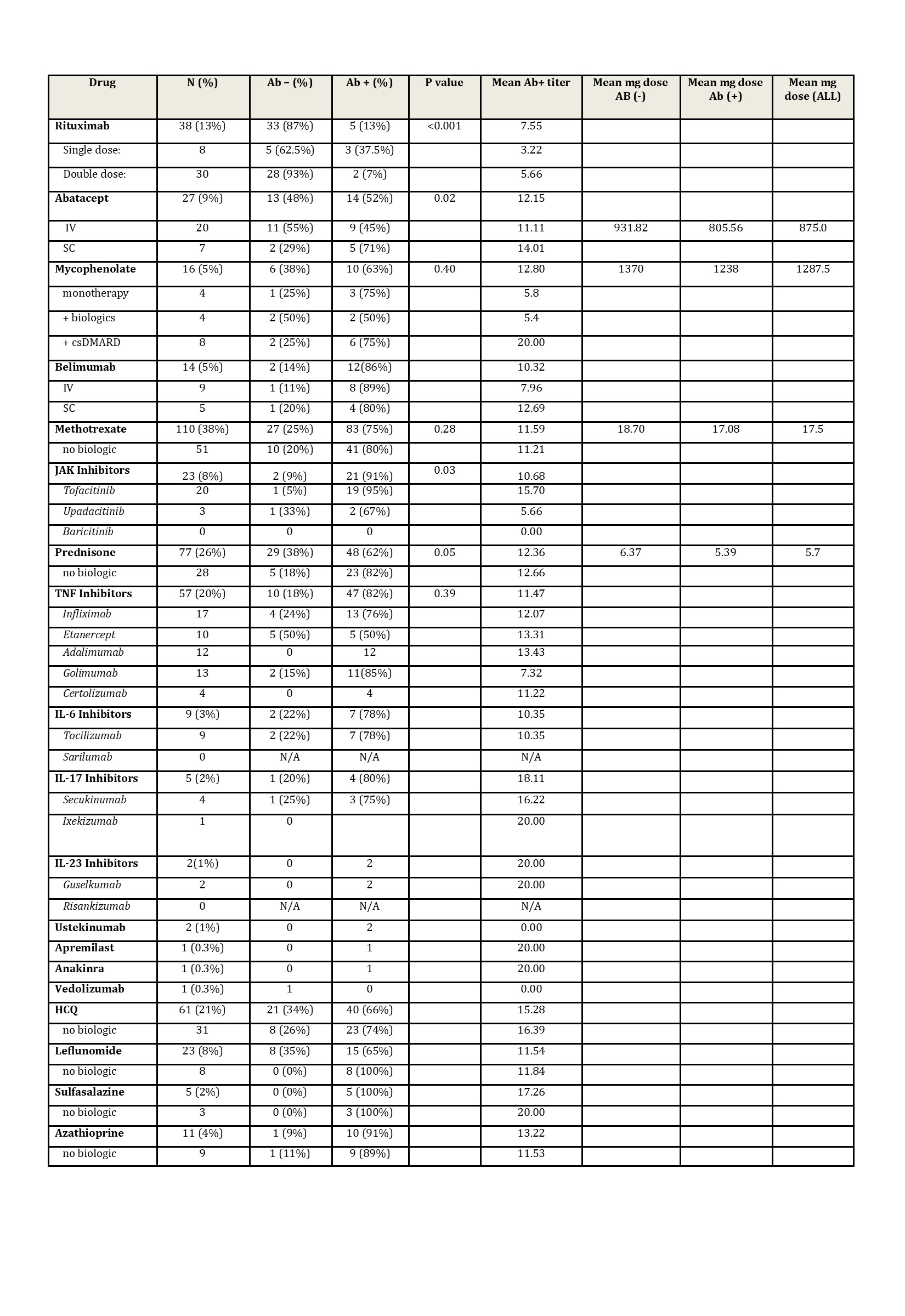
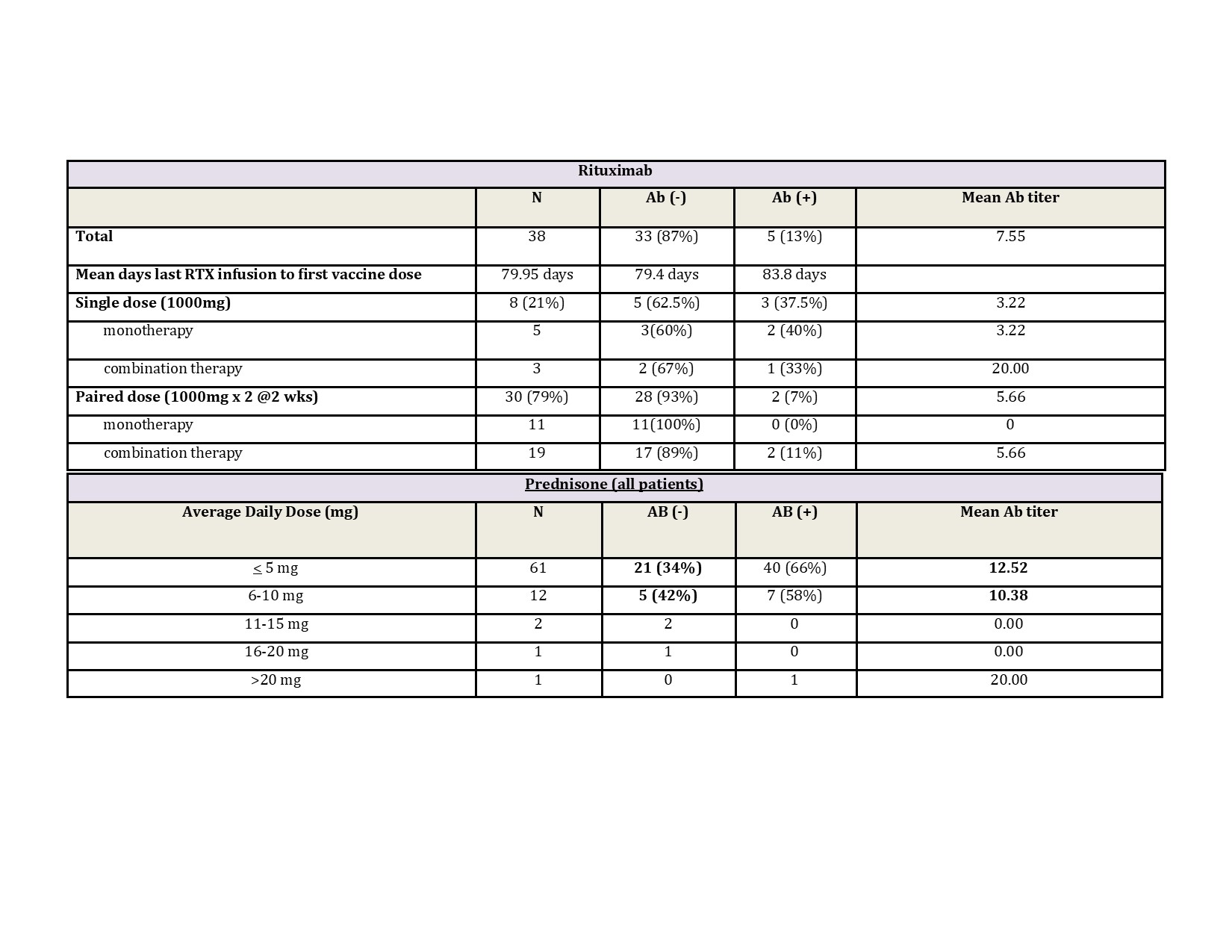
Treatment associations are listed in Table 2. Patients receiving rituximab were less likely to develop an Ab response (13%) and had a lower mean Ab titer (7.55) compared to the overall cohort. Dosing appeared to affect response rates with a single dose (1000 mg) Ab+ rate of 38% compared to a paired dose (1000 mg x2) rate of 7% (Table 3). Patients receiving abatacept IV were also less likely to develop an Ab response (45%). Detectable antibodies were seen in nearly all patients on JAKi (91%), belimumab (86%), TNFi (82%), IL-17i (80%), IL-6i (78%), IL-23i (100%) and IL-12/23i (100%).
Without concomitant targeted therapy, Ab+ rates with mycophenolate (75%) and MTX (80%) were decreased compared to sulfasalazine (100%), leflunomide (100%) and azathioprine (89%). 82% of patients receiving prednisone without biologics were Ab+ (average daily dose <10 mg). Overall dose effect is shown in Table 3.
Conclusion: A majority (71%) of AIIRD patients developed detectable anti-SARS-CoV-2 RBD Abs. Ab response rates and titers were age dependent. Patients receiving rituximab and abatacept IV were less likely to develop an Ab response with the former having a dose effect. Among csDMARDs, response rates were decreased in patients receiving MTX and mycophenolate. Low dose prednisone without biologics did not appear to influence Ab+ rates. Limitations of this study include its single center, non-randomized design and lack of residual confounder measures. Additional measures of humoral immune response and T cell function are also needed. However, this real-world study may provide further guidance for COVID-19 vaccination in patients with AIIRDs on immunomodulatory drugs.
To cite this abstract in AMA style:
Lam G, Laster A, McCarter S, Gladue H, Kashif A, Siceloff E, Lackey V, Robertson C, Toci A, Calabrese L. Immunogenicity of COVID-19 Vaccines in Patients with Autoimmune and Inflammatory Rheumatic Diseases (AIIRDs) [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/immunogenicity-of-covid-19-vaccines-in-patients-with-autoimmune-and-inflammatory-rheumatic-diseases-aiirds/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/immunogenicity-of-covid-19-vaccines-in-patients-with-autoimmune-and-inflammatory-rheumatic-diseases-aiirds/