Session Information
Date: Monday, November 9, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Bench to Bedside
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Recent reports indicate that autoreactive anti-dsDNA IgE autoantibodies and IgE immune complexes and can activate innate and adaptive immunity leading to amplification of lupus immune dyeregulation including induction of type I Interferon (IFN) responses. The aim of this study is to understand the differences in long-term outcomes of SLE patients with or without IgE autoantibodies with high vs. low IFN gene score at baseline.
Methods: The study included 95 adult SLE subjects who fulfilled the 1997 ACR SLE criteria and were enrolled in an IRB approved long-term natural history study. In addition to clinical evaluation, Safety of Estrogen in Lupus National Assessment – SLE Disease Activity Index (SELENA-SLEDAI) scores were recorded at baseline, 36, 60, and 84 month follow-up periods. Anti-dsDNA-IgE autoantibodies were measured by ELISA and a 21-Type I IFN inducible gene composite score was derived from whole blood RNA sequencing at baseline. A high IFN score was defined as an IFN score of >4. The patients were divided into four groups: IgE-positive/high IFN score, IgE-positive/low IFN score, IgE-negative/high IFN score, and IgE-negative/low IFN score. SLE flare was defined as an increase of ≥4 points in the SELENA-SLEDAI score. The locally weighted scatter plot smoother (LOESS) curves were generated for each group to identify longitudinal trends in SELENA-SLEDAI scores. Wilcoxon ranked sum test was used to compare the IgE-positive subjects with the IgE-negative subjects, and to compare the IgE-positive/high IFN score with IgE-negative/low IFN score subjects.
Results: The clinical and demographic features of the SLE subjects are shown in Table 1. Patients with IgE anti-dsDNA antibodies (n=28) were found to have high IFN scores (p=0.012). The IgE-positive group had higher SELENA-SLEDAI scores at baseline and during follow-up (p values, < 0.001, 0.008 and 0.04, at baseline, 60 and 84 months, respectively) (Fig 1). The subset of patients with anti-dsDNA-IgE-positive/high IFN score(n=17) were found to have significantly higher baseline SELENA-SLEDAI scores that remained elevated during the study period (p values, < 0.001, 0.03, 0.07 and 0.009 at baseline, 36, 60 and 84 month, respectively) (Fig 2). The IgE-negative/Low IFN score group (n=45) had the lowest SLE disease activity compared to the other groups (47.7% vs. 64.7%, p=0.09) and the longest flare-free interval (74 months) when compared to the other groups.
Conclusion: SLE patients that are positive for anti-dsDNA-IgE autoantibodies display higher lupus disease activity and IFN scores compared to the anti-dsDNA-IgE negative group. A combination of IgE positive antibodies and high IFN score is associated with significantly enhanced lupus disease activity during longterm follow-up. Our study suggests that presence of IgE autoantibodies and elevated IFN gene score represents a subset of patients with persistently active disease despite standard of care. As omalizumab, a monoclonal antibody against IgE, can modulate type I IFN responses, this study further supports that strategies that target IgE autoantibodies may benefit specific subgroups of SLE subjects.
Acknowledgement: This research was supported by the Intramural Research Program of the NIAMS/NIH.
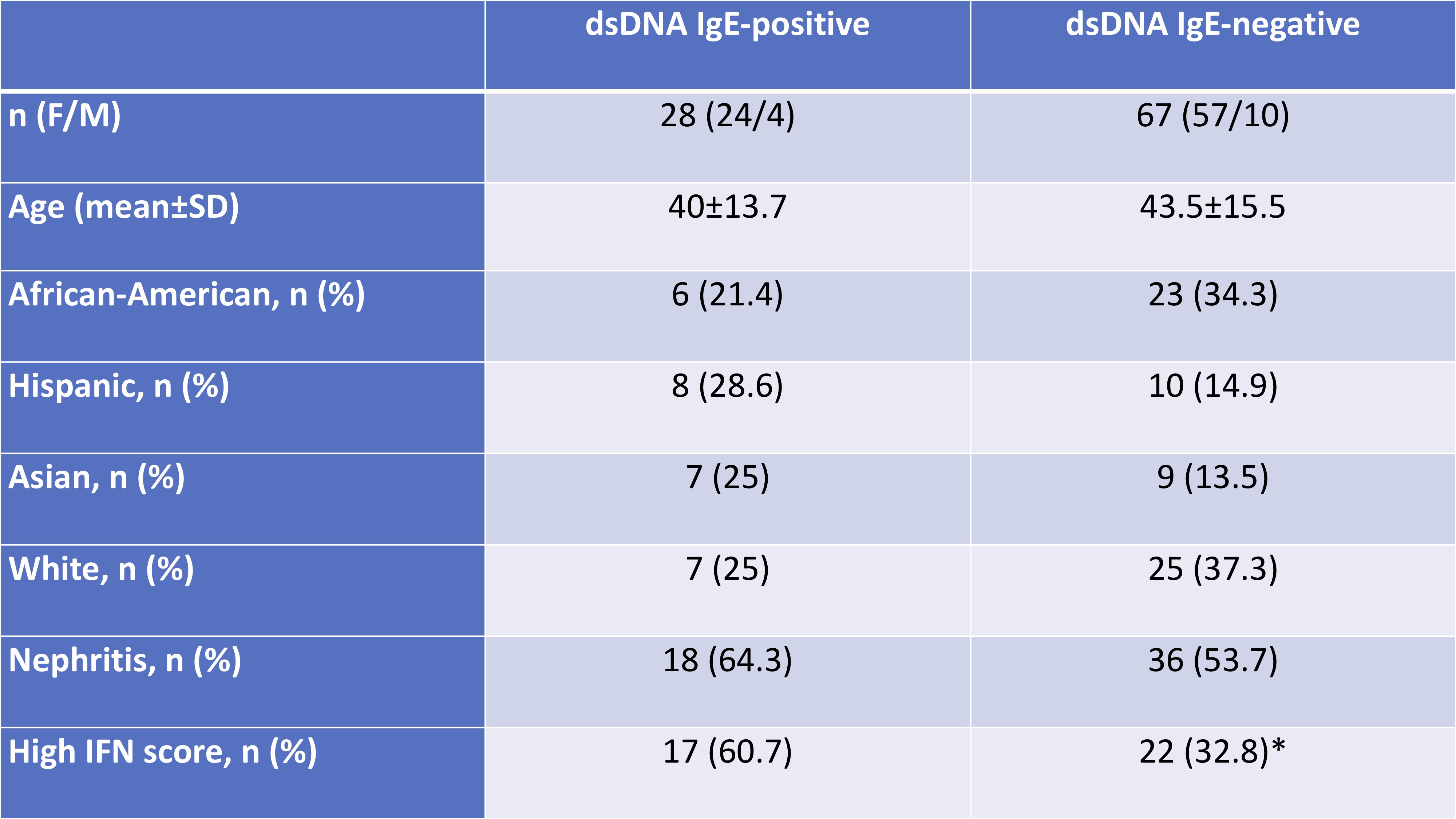 Demographic and clinical features of the SLE patients.
Demographic and clinical features of the SLE patients.
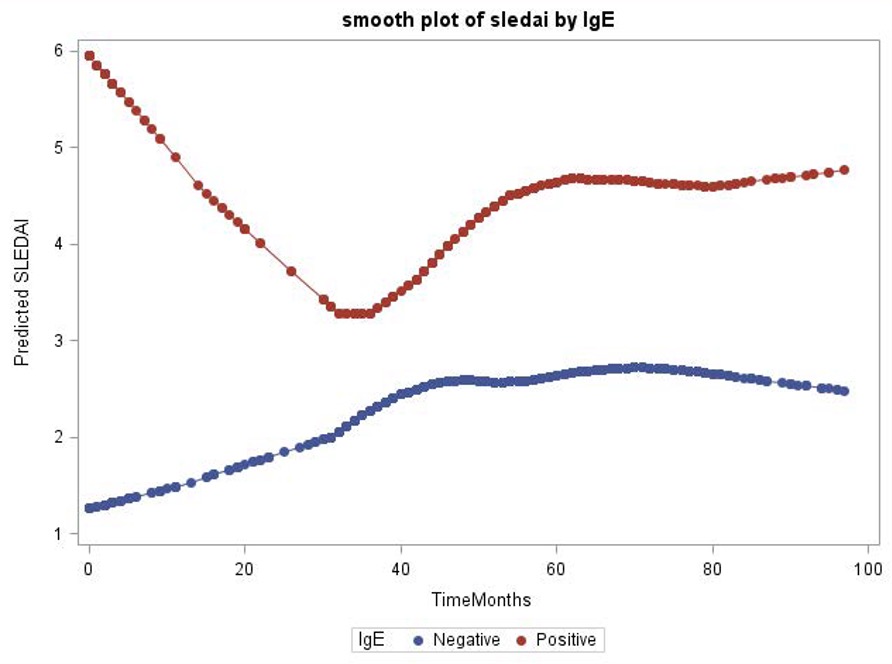 SELENA-SLEDAI scores of patients during the study by dsDNA-IgE autoantibody.
SELENA-SLEDAI scores of patients during the study by dsDNA-IgE autoantibody.
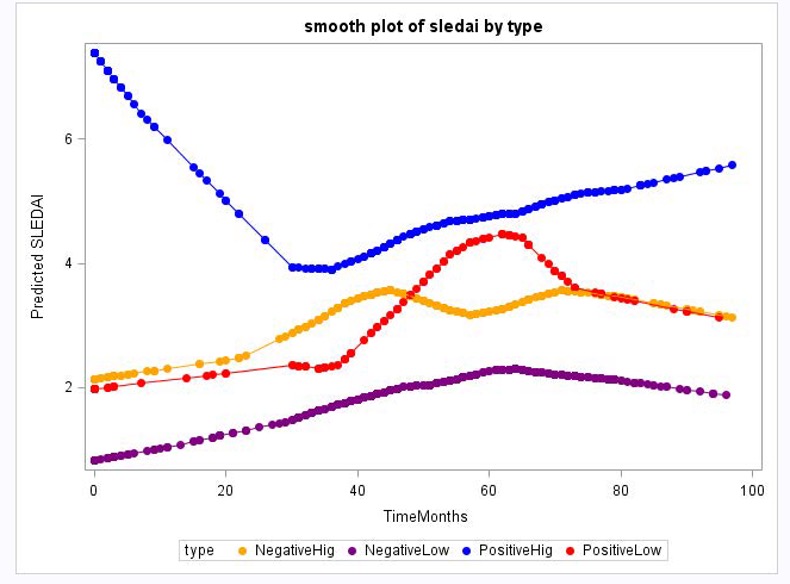 SELENA-SLEDAI scores of patients by dsDNA-IgE autoantibody and IFN score.
SELENA-SLEDAI scores of patients by dsDNA-IgE autoantibody and IFN score.
To cite this abstract in AMA style:
Pamuk O, Manna Z, Adhanom R, Li X, Kaplan M, Hasni S. IgE Anti-dsDNA Antibodies in Systemic Lupus Erythematosus Are Associated with Higher Disease Activity at the Baseline and in Longterm Follow-up [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/ige-anti-dsdna-antibodies-in-systemic-lupus-erythematosus-are-associated-with-higher-disease-activity-at-the-baseline-and-in-longterm-follow-up/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ige-anti-dsdna-antibodies-in-systemic-lupus-erythematosus-are-associated-with-higher-disease-activity-at-the-baseline-and-in-longterm-follow-up/
