Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Despite DMARD treatment, many RA patients continue to suffer from pain. Defining distinct pain phenotypes may advance the use of therapies targeted at specific pain mechanisms. This study identified pain profiles among RA patients with active disease, with the goal of informing treatment decisions to improve pain outcomes.
Methods: 146 RA patients with active disease were identified from 5 academic medical centers. Trained assessors performed joint and tender point counts. Patient-reported measures of pain, fatigue, sleep and psychological distress were assessed. Quantitative sensory testing was done to evaluate pain sensitivity (pressure pain thresholds), central pain sensitization (temporal summation) and descending pain inhibition (conditioned pain modulation). A principle components analysis (PCA) was performed to identify variables explaining the most variance. These variables were used in a hierarchical cluster analysis to identify pain phenotypes. General linear and logistic regression models were used to identify differences in clinical characteristics.
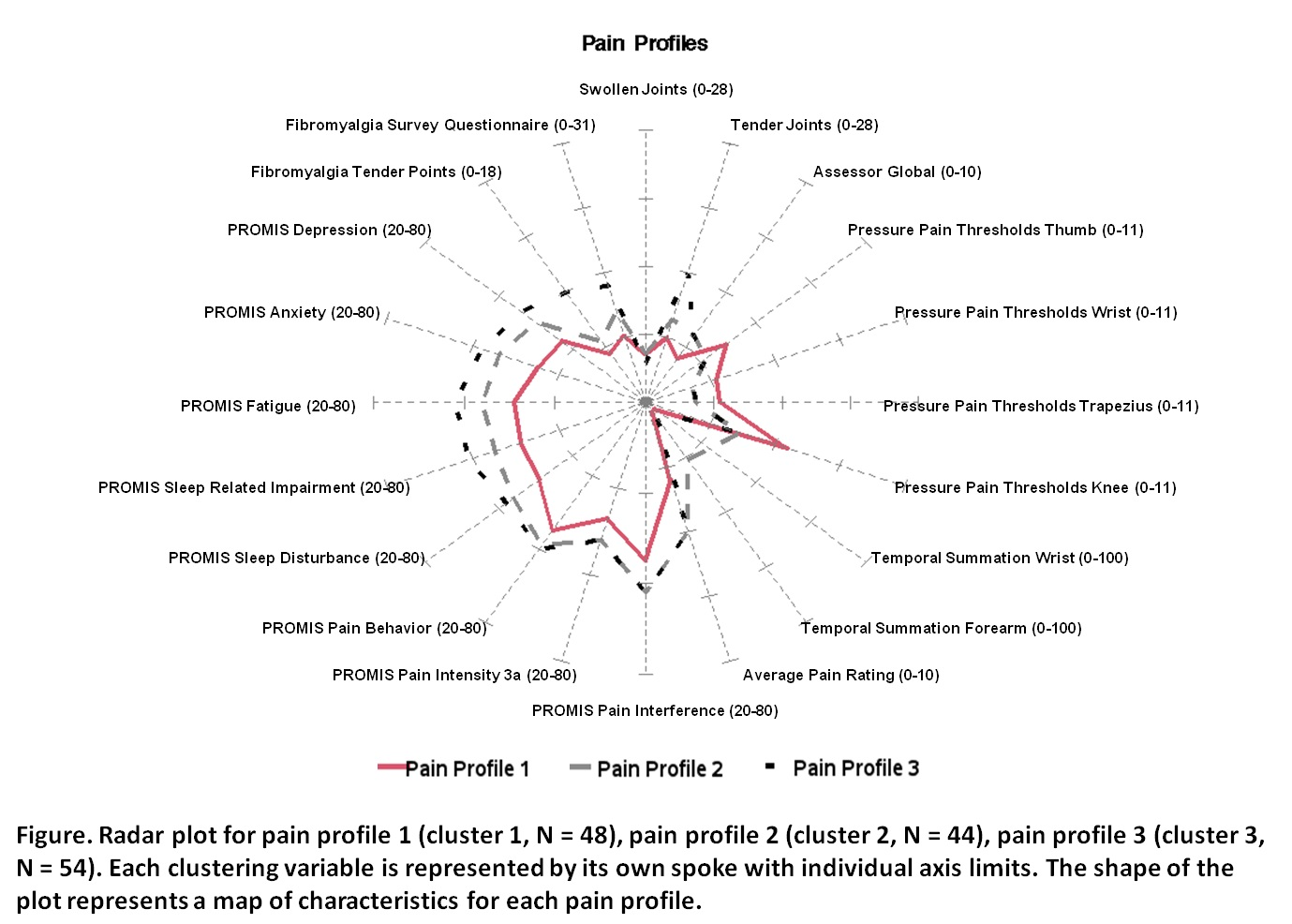
Results: Based on PCA, 20 variables were included in the cluster analysis, which identified 3 pain profiles (Figure): 1) low pain and temporal summation with low psychological distress, fatigue, and sleep problems (N = 48, 32.9%); 2) moderate pain and high temporal summation with moderate psychological distress, fatigue, and sleep problems (N = 44, 30.1%) and 3) moderate pain and temporal summation with high psychological distress, fatigue and sleep problems (N = 54, 37.0%). Catastrophizing and patient global differed across groups, with the low pain group (cluster 1) having the lowest levels of both (Table). NSAID use differed across groups, with the highest frequency of use in the high temporal summation group (cluster 2). Disease duration, CRP and swollen joint count did not differ across groups.
Conclusion: Among RA patients with active disease, 3 pain phenotypes emerged that may inform treatment decisions. Patients with moderate pain and high temporal summation (cluster 2) may benefit from strategies to reduce central sensitization, whereas patients with moderate pain and high psychological distress/fatigue/sleep problems (cluster 3) may benefit from treatments to improve mood and sleep. The finding that NSAID use was highest in the group with high temporal summation is interesting, given a study showing that COX-2 inhibition decreases temporal summation and improves pain (Arendt-Nielsen 2016). Future studies are needed to determine the role of pain phenotypes in directing pain management.
To cite this abstract in AMA style:
Wohlfahrt A, Zhang Z, Lu B, Bingham III CO, Bolster MB, Marder W, Moreland LW, Phillips K, Neogi T, Lee YC. Identification of Clinically Relevant Pain Profiles in Individuals with Active RA [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/identification-of-clinically-relevant-pain-profiles-in-individuals-with-active-ra/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identification-of-clinically-relevant-pain-profiles-in-individuals-with-active-ra/