Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Methods: Using a United Kingdom general population database, we conducted an incident user study of adult SLE patients, identified by Read codes, who initiated HCQ between January 1, 1996 and December 31, 2015. We examined the secular trend of the proportion of initial prescribed HCQ doses exceeding 6.5mg/kg/day IBW as well as 5mg/kg/day ABW and assessed whether excess doses according to these guidelines varied by age, sex, body mass index (BMI; lean, overweight, and obese), and chronic kidney disease (CKD; defined by a eGFR <60).
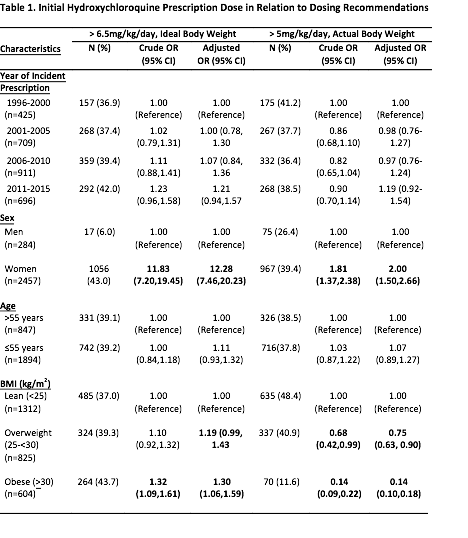
Results: Of 2741 SLE patients who initiated HCQ over this 20-year period, 36.2% of the prescribed doses were > 6.5mg/kg/day IBW, and 38.12% were > 5mg/kg/day ABW. There was no significant change in the rate of initial excess dosing over time for either dose cut-off (p for trends=0.09 and 0.25, respectively) (Table 1). Women had an increased risk of excess initial dosing compared with men, with OR=12.28 (95% CI, 7.46-20.23) for IBW and 2.00 (95% CI, 1.50- 2.66) for ABW dose recommendations. Obesity was associated with a lower risk of excess HCQ dosing using ABW (OR 0.14 for obese vs. lean (95% CI, 0.10-0.18), and a higher risk of excess dosing using IBW (OR 1.30 [95% CI, 1.06-1.59]). Age had no effect on the risk of excess HCQ dosing according to either recommendation (OR 1.11; 95% CI, 0.93-1.32 for IBW, and OR=1.07, 95% CI, 0.89-1.27 for ABW). For the subgroup with available eGFR data (n=657), CKD was associated with an increased risk of excess dosing per ABW (OR 1.85, 95% CI, 1.02-3.37) after adjusting for BMI.
Conclusion: In this general population-based study, over one-third of SLE patients were initiated on HCQ doses exceeding both dosing guidelines, and these rates have not changed over the past two decades. This rate of excess dosing is strikingly higher among women. Obesity posed opposing risk of excess dosing between the two weight-based dosing guidelines. Furthermore, excess dosing is also higher amongst CKD patients per the recent ABW-based guidelines. These findings highlight the potential need to improve excess HCQ dosing, and call for unifying, robust, and evidence-based recommendations.
To cite this abstract in AMA style:
Jorge A, Lu L, Zhang Y, Rai SK, Young LH, Melles RB, Marmor MF, Costenbader KH, Ramsey-Goldman R, Lim SS, Esdaile JM, Clarke AE, Urowitz M, Askanase A, Aranow C, Petri M, Choi HK. Hydroxychloroquine Initiation Dosing Trends and Predictors in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/hydroxychloroquine-initiation-dosing-trends-and-predictors-in-systemic-lupus-erythematosus/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hydroxychloroquine-initiation-dosing-trends-and-predictors-in-systemic-lupus-erythematosus/