Session Information
Date: Tuesday, November 12, 2019
Title: 5T093: SLE – Clinical V: Emerging Knowledge of Current Treatments (2780–2785)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: The antimalarial drug hydroxychloroquine (HCQ) has a primary role in the treatment of systemic lupus erythematous (SLE). Beyond its pleiotropic immunomodulatory effects on TLR and type I interferon signaling, HCQ use has been found to be protective for thrombosis in SLE. Optimal dosing of HCQ in SLE is unknown. The longitudinal measurement of HCQ blood levels may provide an opportunity to individualize weight-based dosing strategies and reduce risk of toxicity. We examined the association of HCQ blood levels with thrombotic events in a longitudinal SLE cohort.
Methods: Patients with no HCQ level measured prior to the thrombosis were excluded. 812 SLE patients were included: 93% female, 43% African-American, 46% Caucasian. HCQ blood levels were quantified by liquid chromatography-tandem mass spectrometry. Mean HCQ blood levels (± SD) over all cohort visits prior to occurrence of thrombosis were calculated for each patient. Thromboses were defined as venous (DVT/PE or other venous) or arterial thrombosis (stroke, myocardial infarction, digital gangrene or other arterial).
Results: Thrombosis had occurred during prospective follow up in 44 patients (5.4%), venous in 3.0% and arterial in 2.5%. Lupus anticoagulant was strongly associated with a history of any thrombosis (OR 3.25, P< 0.0001), venous thrombosis (OR 3.53, P< 0.0001), and arterial thrombosis (OR 3.08, P< 0.0001). A prospective analysis (Table 1) shows that for any thrombosis and for venous thrombosis, the HCQ blood level was significantly lower. Higher prescribed doses of HCQ (as opposed to HCQ blood levels) were also associated with decreased odds of any thrombosis and also of venous thrombosis (Table 2) in a separate cross-sectional analysis (OR 0.88, P=0.04 and OR 0.83, P=0.009, respectively for each 1 mg/kg increase in prescribed HCQ).
Conclusion: HCQ blood levels are inversely associated with risk of any thrombosis and of venous thrombosis in patients with SLE in a prospective analysis. Reduction of HCQ dosing, as suggested by the American Academy of Ophthalmologists, could reduce or eliminate the benefit of hydroxychloroquine to prevent thrombosis.
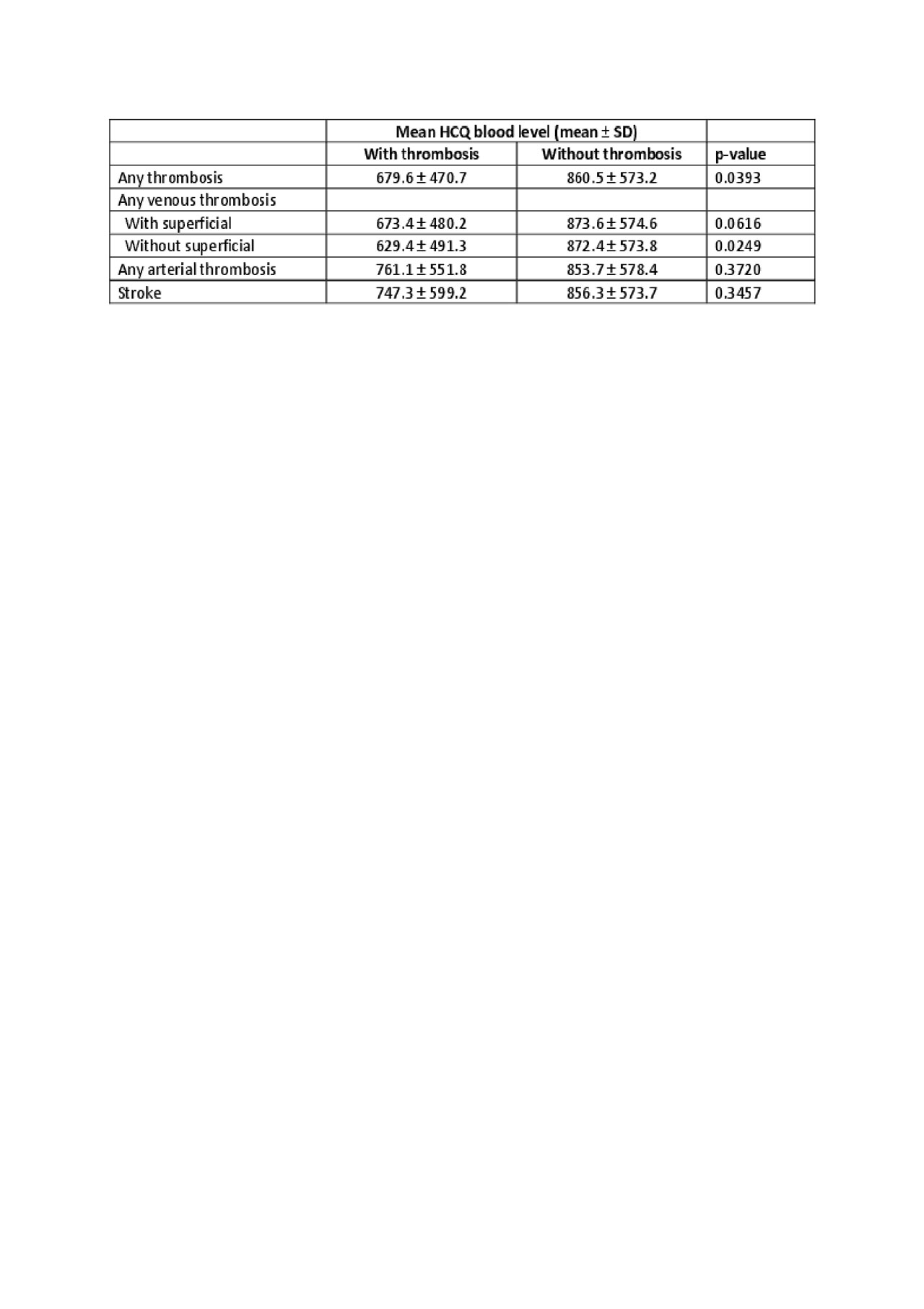
ACR 2019 Abstract HCQ and Thrombosis-Konig v3-Table1

ACR 2019 Abstract HCQ and Thrombosis-Konig v3-Table2
To cite this abstract in AMA style:
Konig M, Li J, Petri M. Hydroxychloroquine Blood Levels and Risk of Thrombotic Events in Systemic Lupus Erythematous [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/hydroxychloroquine-blood-levels-and-risk-of-thrombotic-events-in-systemic-lupus-erythematous/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hydroxychloroquine-blood-levels-and-risk-of-thrombotic-events-in-systemic-lupus-erythematous/
