Session Information
Date: Monday, November 13, 2023
Title: (1345–1364) Reproductive Issues in Rheumatic Disorders Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Adolescent and young adults (AYAs) with rheumatic disease (RD) may face disproportionate risk of HPV and associated cancers due to immune dysregulation, immunosuppression and gaps in preventive health care delivery. As vaccination is a safe and effective means of prevention, we aimed to evaluate whether having an RD is associated with decreased HPV vaccine uptake in AYAs seen by a rheumatologist.
Methods: This retrospective study included individuals aged 16-22 seen in our academic rheumatology center ≥2 times (2020-2022) with New York State (NYS) residence. We used chart review to ascertain demographics, vaccine information (automatically pulled from the NYS Immunization Information System), reason for evaluation by a rheumatologist, and medication information. We descriptively compared demographic and clinical variables between patients with and without an RD diagnosis. We performed a multivariable logistic regression to assess whether having an RD diagnosis was associated with having received 2-3 HPV vaccine doses after adjusting for relevant demographic characteristics and receipt of other elective vaccines.
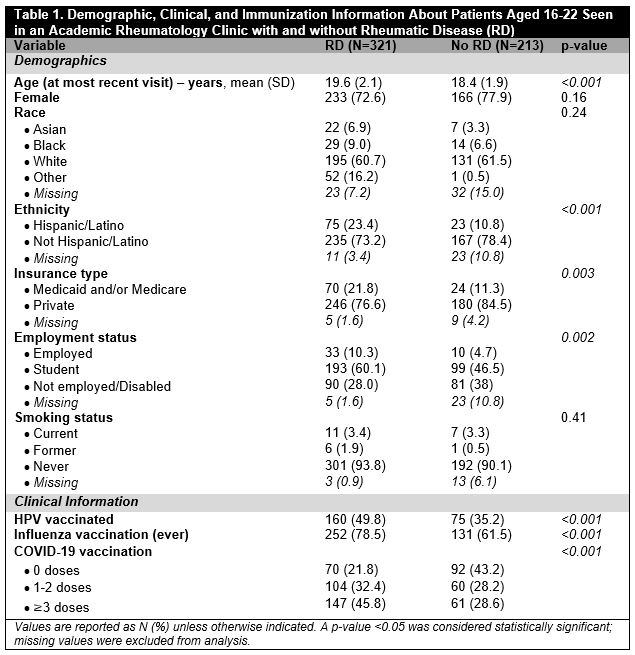
Results: There were 534 patients aged 16-22 seen by a rheumatologist at our center ≥2 times during the study period with NYS residence (mean age ± 2.1 years, 74.7% female, and 61% White). Compared to those without RD (n=213), patients with RD (n=321) were older (mean age 19.6 vs. 18.4 years, p< 0.001), more frequently Hispanic/Latino (23.4% vs. 10.8%, p< 0.001), more had Medicaid and/or Medicare (21.8% vs. 11.3%, p=0.003), more were employed (10.3% vs. 4.7%) and students (60.1% vs. 46.5; p=0.002) [Table 1].
Overall, 235 (44%) patients were HPV vaccinated (49.8% with RD vs. 35.2% without RD, p< 0.001). Compared to non-RD patients, those with RD were more likely to have ever received the influenza vaccine (78.5% vs. 61.5%, p< 0.001) and ≥3 doses of the COVID-19 vaccine (45.8% vs. 28.6%, p< 0.001) [Table 1]. Of 321 patients with RD, 86.9% were diagnosed with inflammatory arthritis or CTD; 61.4% were diagnosed with RD before age 17 [Table 2].
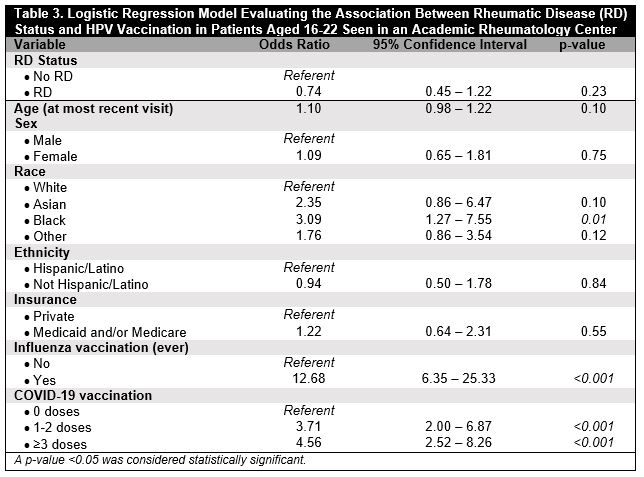
In adjusted models, RD status was not associated with HPV vaccination (OR 0.74, 95% CI 0.45-1.22, p=0.23). Black vs. White race was associated with HPV vaccination (OR 3.09, 95% CI 1.27-7.55, p=0.01). Influenza vaccination (ever) (OR 12.68, 95% CI 6.35-25.33, p< 0.001) and COVID-19 vaccination (OR 3.71 for 1-2 vs. 0 doses, 95% CI 2.00-6.87, p< 0.001; OR 4.56 for ≥3 vs. 0 doses, 95% CI 2.52-8.26, p< 0.001) were associated with HPV vaccination [Table 3].
Conclusion: Among AYAs seen in an academic rheumatology center, less than half were HPV vaccinated, and having an RD was not associated with HPV vaccination in adjusted models. Receipt of HPV and other elective vaccines was more common for patients diagnosed with an RD compared to those who were not. Influenza vaccination (ever) was associated with 13-fold increased likelihood of HPV vaccination, and COVID-19 vaccination (≥3 doses) with 5-fold increased likelihood of HPV vaccination, after adjusting for relevant factors. Interventions are needed to improve HPV vaccine uptake in AYAs, including those with RD at increased risk of vaccine-preventable illnesses; targeting elective vaccine uptake in general may be a fruitful approach.
To cite this abstract in AMA style:
Siegel C, Robinson L, Jannat-Khah D, Mikhaylov A, Pan N, Sammaritano L. HPV Vaccination in Adolescent and Young Adult Patients Seen in an Academic Rheumatology Center [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/hpv-vaccination-in-adolescent-and-young-adult-patients-seen-in-an-academic-rheumatology-center/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hpv-vaccination-in-adolescent-and-young-adult-patients-seen-in-an-academic-rheumatology-center/