Session Information
Date: Sunday, October 21, 2018
Title: Rheumatoid Arthritis – Treatments Poster I: Strategy and Epidemiology
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: After failure of initial methotrexate (MTX) treatment in rheumatoid arthritis (RA) patients, various treatment options can be considered. To date, evidence about the preferred follow-up strategy is sparse. We aimed to compare consecutive DMARD treatment regimes in daily practice in RA patients who failed on initial MTX monotherapy.
Methods: Newly diagnosed RA patients who had failed initial MTX treatment were selected from METEOR, an international, observational registry. Subsequent DMARD treatment regimens were categorized as: 1) csDMARD(s) only (143 patients), 2) csDMARD(s) + glucocorticoid (278 patients) and 3) bDMARD ± csDMARD(s) (89 patients). We selected follow-up visits until switch to yet another treatment strategy occurred or until a maximum follow-up duration of 1 year. Linear mixed model analyses were performed to analyze treatment responses per treatment group (DAS) after a maximum follow-up duration of 6 and 12 months. Differences in time to stop treatment between treatment groups after a maximum follow-up duration of 1 year were estimated using Cox regression. Analyses were adjusted for multiple propensity scores, to correct for confounding by indication.
Results: Median follow-up duration on studied treatment was 6.9 (IQR 4.1; 9.4) months for patients receiving csDMARD(s), 7.8 (IQR 5.0; 10.2) months for patients receiving csDMARD(s) + glucocorticoid and 9.0 (IQR 6.2; 10.9) months for patients receiving treatment including a bDMARD.
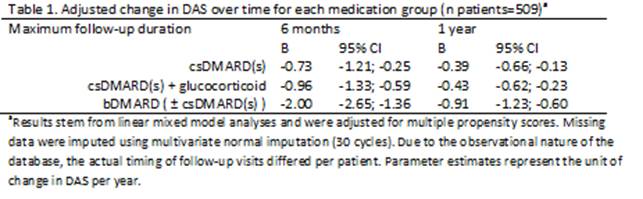
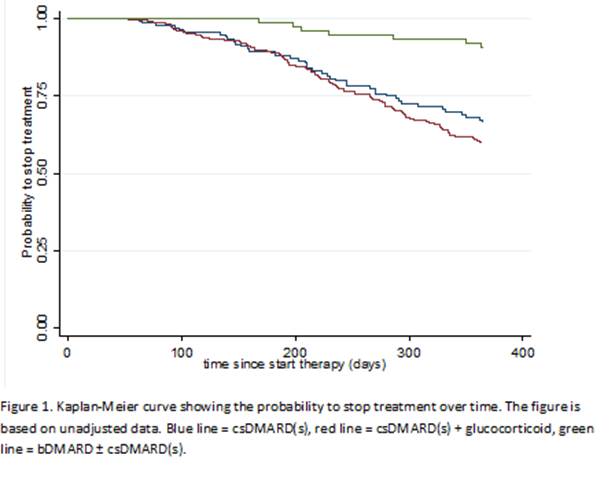
We found differences in treatment response between the 3 treatment groups, both after 6 months (p=0.001) and after 1 year (p=0.029). Adjusted treatment effects over time stratified for treatment groups are shown in table 1. Both after 6 months and after 1 year, patients receiving a bDMARD experienced most decrease in DAS per year, followed by patients receiving csDMARD(s) + glucocorticoid and by patients receiving treatment with csDMARD(s) alone. Results of the Cox regression showed that patients receiving treatment including a bDMARD had a lower hazard for discontinuing treatment (i.e. failing or intolerance) compared to patients receiving csDMARD(s) alone [HR (95% CI) 0.38 (0.24; 0.60)], but there were no differences between csDMARD treatment with- or without a glucocorticoid [HR (95% CI 0.89 (0.66; 1.20), figure 1].
Conclusion: In this analysis of worldwide common practice data, RA patients who had failed initial treatment with MTX monotherapy had a better DAS response and treatment survival after a subsequent switch to a bDMARD containing treatment regimen than to a regiment with csDMARD(s), with or without glucocorticoids.
To cite this abstract in AMA style:
Bergstra SA, Winchow LL, Murphy E, Chopra A, Salomon-Escoto K, Fonseca JE, Allaart CF, Landewé RBM. How to Treat Rheumatoid Arthritis Patients When Methotrexate Has Failed? Results from the Meteor Registry [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/how-to-treat-rheumatoid-arthritis-patients-when-methotrexate-has-failed-results-from-the-meteor-registry/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/how-to-treat-rheumatoid-arthritis-patients-when-methotrexate-has-failed-results-from-the-meteor-registry/