Session Information
Title: Health Services Research, Quality Measures and Quality of Care - Innovations in Health Care Delivery
Session Type: Abstract Submissions (ACR)
Background/Purpose: The American College of Rheumatology (ACR) in 2008 and 2012 published guidelines for the use of disease modifying anti-rheumatic drugs (DMARD) and biologics in rheumatoid arthritis (RA) in an attempt to improve quality and decrease variability in RA care. In addition, in 2012, a unique population management program for RA was initiated in our institution, an academic tertiary center, designed to improve quality and safety while reducing cost of care in RA. The aim of the present project was to characterize the variability in RA care provided in the rheumatology practice in our institution, according the ACR and local measures.
Methods: Data on 80 consecutive patients with newly diagnosed RA between 1/1/2010 and 8/1/2011 with at least 18 month follow-up period were extracted through the electronic health records (EHR). RA diagnosis was made based on ICD-9 code 714.0 by a rheumatologist. Additional data were extracted by manual review of the EHR by four of the authors. The primary objective was to measure practice patterns in RA care and DMARD use according to selected quality measures. Secondary objective was to compare the actual vs. perceived RA care rendered by rheumatologists. For that purpose, we used a survey with questions regarding DMARD use in RA that had been administered earlier to all staff rheumatologists and fellows as part of our population management program. The results of this survey were termed “perceived” care. This was compared to the actual RA care delivered by these providers, based on data extracted from the EHR, termed “actual” care.
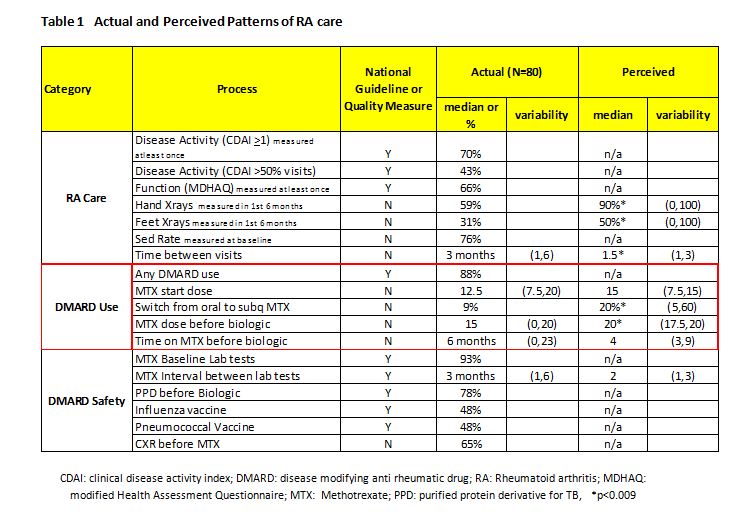
Results: Results are shown in Table 1. We achieved >60% in disease activity and functional measures, DMARD use and PPD before starting a biologic, but <50% in obtaining a disease activity measure in at least 50% of the visits, and administering pneumococcal and influenza vaccinations in patients on DMARDs. MTX median starting dose was 12.5 (min 7.5, max 20) mg/weekly; switch from oral to injectable MTX was only 9%, although physician perception was 20%; and, the median time patients were treated with MTX prior to starting a biologic was 6 (min 1, max 6) months with physician perception being 4 months.
Conclusion: Our results showed there is need for improvement in several selected measures in RA care. Improvement in quality should aim to increase the routine collection of disease activity measures, greater use of injectable MTX and vaccinations. Cost reduction should aim to reduce variability in MTX use prior to starting biologics in terms of both time and dosages and in laboratory monitoring. There were also differences in the perception of rheumatologists about the care they deliver and the actual care that is delivered. Results of this study will be used as a benchmark for ACR measures and our population management program, in order to examine ways to reduce variability and improve quality in the care provided to RA patients.
Disclosure:
S. Mathew,
None;
T. S. Sharma,
None;
O. Quintero,
None;
O. Bailey,
None;
D. Webb,
None;
E. D. Newman,
None;
A. Bili,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/how-are-actual-patterns-of-care-for-a-health-system-in-rheumatology-in-comparison-with-validated-quality-measures/