Session Information
Date: Monday, November 9, 2015
Title: Rheumatoid Arthritis - Clinical Aspects II: Infection, Malignancy and Other Comorbidites in RA
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Rheumatoid
arthritis (RA) and gout are the two most common inflammatory arthritides
in the US and beyond. As hospitalization for these conditions are
known to incur substantial resource use, hospitalization trends and associated costs
could provide critical benchmarks to the field.
Indeed, varying levels of perceived success in their care (including the
effects of new medications) and changing epidemiology (particularly for gout) may
have made a substantial impact over the past several decades; however, no
relevant data are available. To address
this key knowledge gap, we evaluated hospitalization trends between 1993 and
2011 in the US.
Methods:
We used the National Inpatient Sample (NIS), a database representative of
hospitalizations in the US. We studied hospitalization trends of RA and gout
(as the primary/principal discharge diagnosis using ICD-9-CM codes 714.0, 714.2, 714.30-714.33
and 274.0-274.9, respectively) from 1993 through 2011. We used total hospital charge trends as a
proxy for total cost trends, as charge data were available for the entire study
period. Additionally, we analyzed available
cost data during the latest years (2006-2011), as well as the trend of the
number of surgeries of total knee replacement, total hip replacement, and other
major joint surgeries from 2002-2011, where these data were collected in the
NIS.
Results:
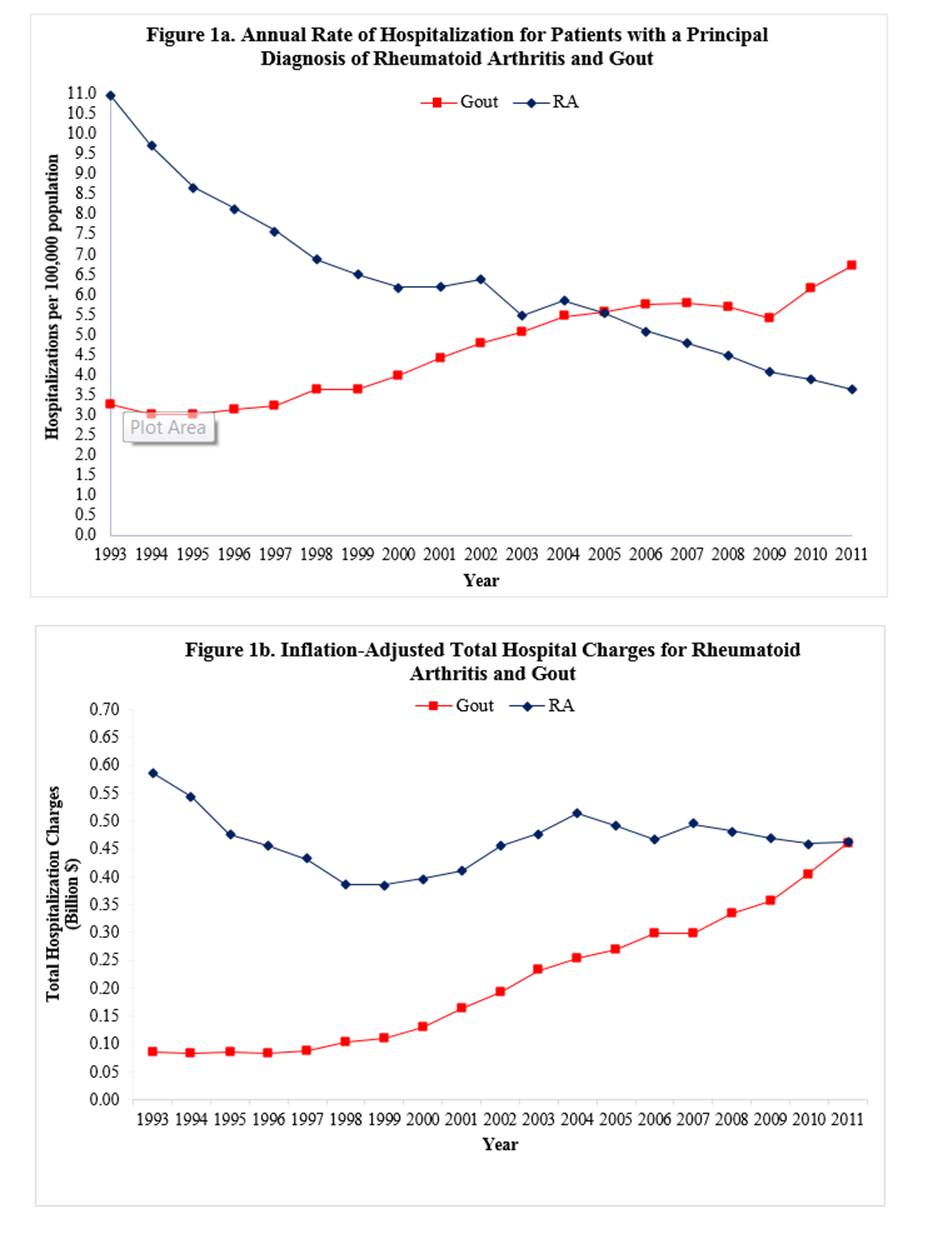
In 1993, admissions for RA were more than 3 times frequent than those for gout
(Figure 1a). From 1993 to 2011, the admission rate for RA
rapidly declined from 10.9 to 3.6 per 100,000 US adults, whereas that for gout
steadily increased from 3.3 to 6.7 per 100,000 US adults, resulting in a reversal
of hospitalization frequency between the two conditions in 2011. Inflation-adjusted total hospital charge trends
for the two conditions reflected the hospitalization trends and became equal in
2011 ($0.46 billion USD) (Figure 1b). The available cost data over the last 6 years
reflected the same trend, resulting in $0.13 billion USD for both conditions. Approximately 70% of RA admissions and 3% of
gout admissions was associated with total joint replacement or other major
joint surgeries from 2002-2011; the trend of the total number of such surgeries
in the two conditions reflected overall hospitalization trends.
Conclusion:
Our findings based on these nationally representative inpatient data indicate
that primary hospitalization rates and the inpatient economic burden for RA
have declined substantially over the past two decades, whereas those for gout
has increased considerably. These strikingly
contrasting trends provide a benchmark for the perceived improvement in RA care
(likely related to the use of biologics), thereby preventing joint
replacements; they also reflect suboptimal gout care in addition to its increasing
prevalence. These data support the need
to improve gout prevention and care.
To cite this abstract in AMA style:
Lim SY, Lu N, Fisher M, Oza A, Rai SK, Menendez ME, Choi H. Hospitalization Trends of Rheumatoid Arthritis and Gout in the United States: A Crossroad [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/hospitalization-trends-of-rheumatoid-arthritis-and-gout-in-the-united-states-a-crossroad/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hospitalization-trends-of-rheumatoid-arthritis-and-gout-in-the-united-states-a-crossroad/