Session Information
Date: Monday, November 6, 2017
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment Poster II: Damage and Comorbidities
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Hospital Readmissions For SLE In The United States: A National Database Study
Background/Purpose: Systemic lupus erythematosus (SLE) is associated with significant mortality and morbidity, and increased hospital readmissions. Data about readmissions among SLE patients on a national level in the United States is sparse. The aim of this study was to describe unplanned hospital readmission rates among adult SLE patients and assess predictors of readmission.
Methods: We analyzed the 2013 National Readmission Database (NRD) to quantify readmission rates among SLE patients. We identified comorbidities and reasons for unplanned 30-day readmissions using administrative codes. We then used survey logistic regression to elucidate predictors for unplanned readmissions using adjusted odds ratios (aOR) and 95% confidence intervals (CI).
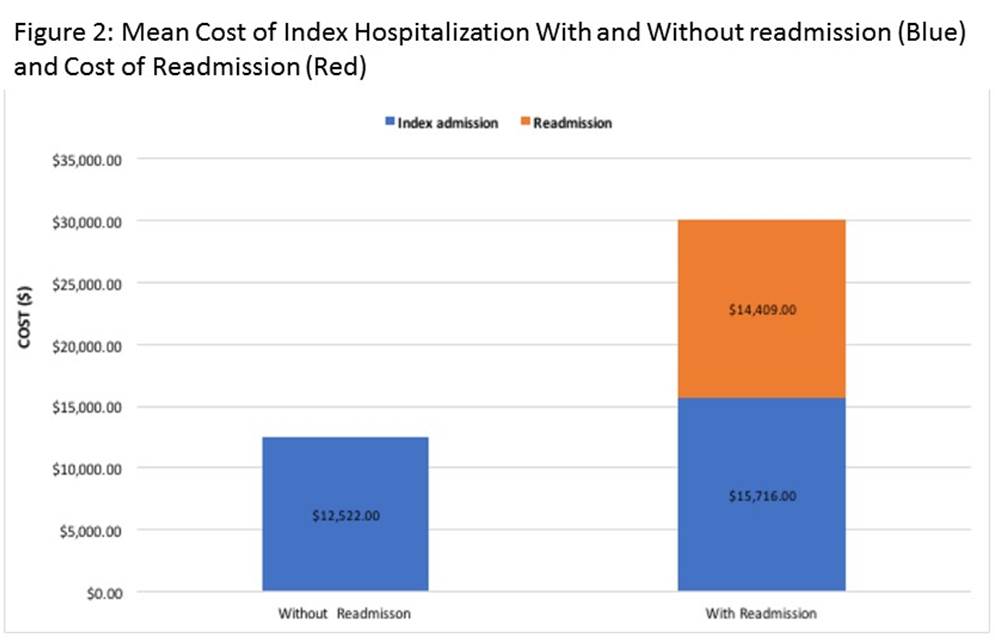
Results: Among 7926 patients with SLE, 1641 had at least one unplanned 30-days readmissions (20.7%). 39% of readmissions were related to SLE (Figure 1A). Readmitted patients were more likely to be young, have glomerulonephritis (GN), chronic kidney disease (CKD), pericarditis, pleuritis, thrombocytopenia and longer length of hospital stay. Significant predictors of SLE included age 18-25 years, CKD, GN, pericarditis, psychosis, anemia, thrombocytopenia, length of stay > 4 days, patients having Medicare and Medicaid insurance, home health care and against medical advice discharges after adjusting for socio-demographics, comorbidities and hospital characteristic (Figure 1). Cost of hospitalization was $12,522 in patients without readmission compared to $15,716 for index admission in patients with readmission (Figure 2). Cost of readmission was an additional $14,409.
Conclusion: In NRD, 20.7% of patients admitted with a primary diagnosis of SLE were readmitted within 30 days. This underscores the importance of close outpatient follow up in the post discharge period especially in high-risk patients with co-morbidities. Readmissions were associated with significant cost.
To cite this abstract in AMA style:
Annapureddy N, Saha A, Nadkarni G. Hospital Readmissions for SLE in the United States: A National Database Study [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/hospital-readmissions-for-sle-in-the-united-states-a-national-database-study/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hospital-readmissions-for-sle-in-the-united-states-a-national-database-study/