Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Prospective cohort studies of pregnancies managed by experts demonstrate that up to 30% of systemic lupus erythematosus (SLE) pregnancies result in preterm birth. We assembled a real-world, multi-center, electronic health record (EHR)-based cohort of SLE births from three tertiary care centers in the Southeastern United States to assess the impact of race on adverse pregnancy outcomes.
Methods: Centers 1 and 2 selected subjects with at least 1 count of the SLE ICD-9 (710.0) or ICD-10 codes (M32.1*, M32.8, M32.9) and at least 1 ICD-9 or ICD-10 code for pregnancy-related diagnoses from 2013-2018. These subjects were reviewed by a rheumatologist to determine if the subject had SLE. Pregnancy outcomes were extracted as discrete variables through the EHR. Center 3 subjects had at least 4 counts of the SLE ICD-9 code or ICD-10 codes and at least 1 ICD-9 or ICD-10 code for pregnancy-related diagnoses. A subject was defined as a case if diagnosed with SLE by a rheumatologist, nephrologist, or dermatologist. Pregnancy outcomes were assessed through chart review for deliveries from 1993-2017. Only pregnancies that delivered at the academic center, had available pregnancy outcomes, and occurred after SLE diagnosis were included. Age-adjusted logistic regression models measured the association of maternal race with preterm birth and preeclampsia.
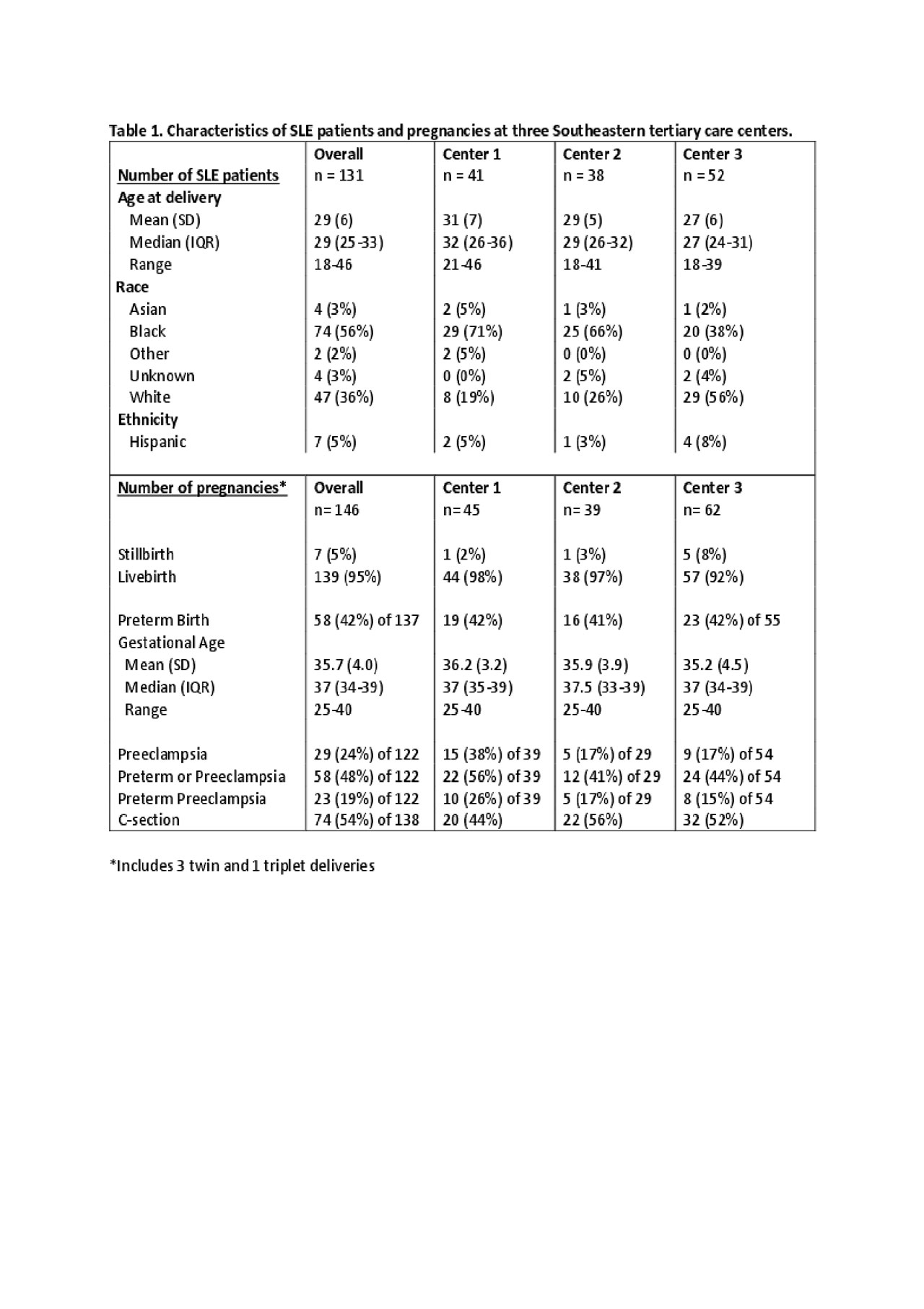
Results: Across the 3 centers, there were 131 women with SLE with 146 pregnancies. The mean age at delivery of 29 years was similar across the 3 centers (Table 1). The demographics were different between centers with more Black women at Center 1 (71%) and 2 (66%) compared to Center 3 (38%); there were very few Hispanic women. Overall, the rate of preterm birth was 42% with a mean gestational age of 35.7 weeks, which was similar in each center. More than half (54%) of all pregnancies were delivered surgically. Preeclampsia complicated 24% of all pregnancies, with the rate of preeclampsia twice as high in Center 1 (38%) compared to Centers 2 and 3 (17%). The large majority of preeclamptic deliveries occurred preterm (79%). When adjusting for maternal age, Black race was not significantly associated with preterm birth (OR = 1.28, 95% CI 0.62 – 2.62, p = 0.5) or preeclampsia (OR = 1.66, 95% CI 0.65 – 4.26, p = 0.3).
Conclusion: We observed higher than previously reported rates of preeclampsia, preterm birth, and Caesarean section at all 3 centers. Only slightly more than half of the deliveries were term and without preeclampsia. In the general population, preeclampsia is most common at term, whereas in this cohort 79% of preeclampsia occurred preterm. These findings likely reflect the severity of disease seen at large tertiary care referral centers in the Southeastern US. While the proportion of pregnancies to Black women was higher in this cohort than others, multivariate analysis demonstrated that race was not associated with adverse outcomes. We hypothesize that these findings reflect referral bias of the sickest SLE patients of all races to deliver at a tertiary care center. Our findings demonstrate that even at specialized, tertiary care centers, there is an unmet need for management guidelines that reduce adverse pregnancy outcomes in SLE.
To cite this abstract in AMA style:
Blaske A, Eudy A, Kirchoff K, Oates J, Clowse M, Barnado A. Higher Than Expected Rates of Adverse Pregnancy Outcomes in Patients with Systemic Lupus Erythematosus from Three Tertiary Care Centers [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/higher-than-expected-rates-of-adverse-pregnancy-outcomes-in-patients-with-systemic-lupus-erythematosus-from-three-tertiary-care-centers/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/higher-than-expected-rates-of-adverse-pregnancy-outcomes-in-patients-with-systemic-lupus-erythematosus-from-three-tertiary-care-centers/